Infection
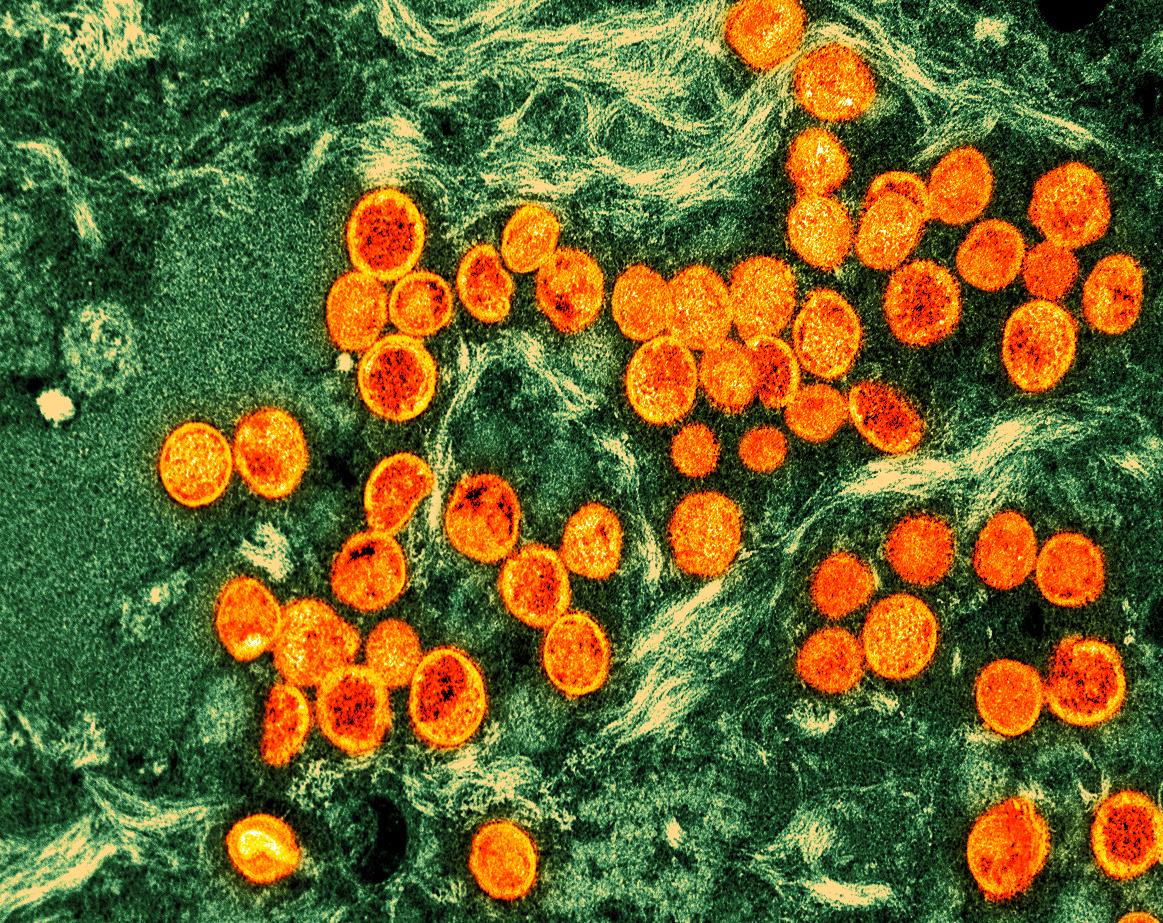
Many mpox patients have other sexually transmitted infections, study shows
A large proportion of mpox patients in Chicago last year and early this year also had other sexually transmitted infections (STIs) such as HIV, predisposing them to severe mpox and potentially contributing to spread of the virus, finds a study led by Chicago Department of Public Health researchers.
The findings, published today in the Journal of Infectious Diseases, involved estimating rates of HIV and other STIs (in this case, gonorrhea and chlamydia) among 1,124 mpox patients from June 2022 to March 2023 and identifying factors tied to mpox severity. Median age was 34 years, 36% were White, 30% were Hispanic, 29% were Black, 92% were cisgender, and 83% of 806 who reported partner sex said they had a male partner.
A multicountry mpox outbreak began in nonendemic countries in May 2022, with most cases in men who have sex with men (MSM). Cases continue to be identified in Chicago, the researchers noted. Advanced HIV is tied to mpox-related hospital admissions and death, and those with weakened immune systems may be more likely to spread the virus to others.
Concurrent HIV tied to hospitalization, death
Of the 1,124 mpox patients, 44% had HIV, and 70% had a previous or current STI, with 39% having had at least three previous STI episodes. Relative to mpox patients who didn’t have HIV, more HIV-infected mpox patients were hospitalized (10.3% vs 4.1%). A total of 76 (7%) of patients were hospitalized—66% of them HIV patients—and all 3 patients who died had advanced HIV.
STI screening visits are opportunities to vaccinate against mpox and provide HIV prophylaxis or treatment.
Of 335 vaccinated mpox patients, 55% had received one dose of the Jynneos vaccine, and 45% had received two. In total, 17.6% were vaccinated before mpox infection, and 2% had received two doses.
“STI screening visits are opportunities to vaccinate against mpox and provide HIV prophylaxis or treatment,” the study authors wrote. “Future research should examine predictors of mpox infection among those with STIs, including other STIs, such as syphilis, HIV risk at STI screening or anatomical site of infection.”