Infection
CDC reviewing morning-after pill for STIs
LOS ANGELES — For the past two and a half years, Rick Turpin has worked at Men’s Health Foundation in West Hollywood as a community embedded disease intervention specialist (CEDIS). His goal — to educate, test, and treat folks in the LGBTQ+ community when it comes to sexually transmitted infections (STIs).
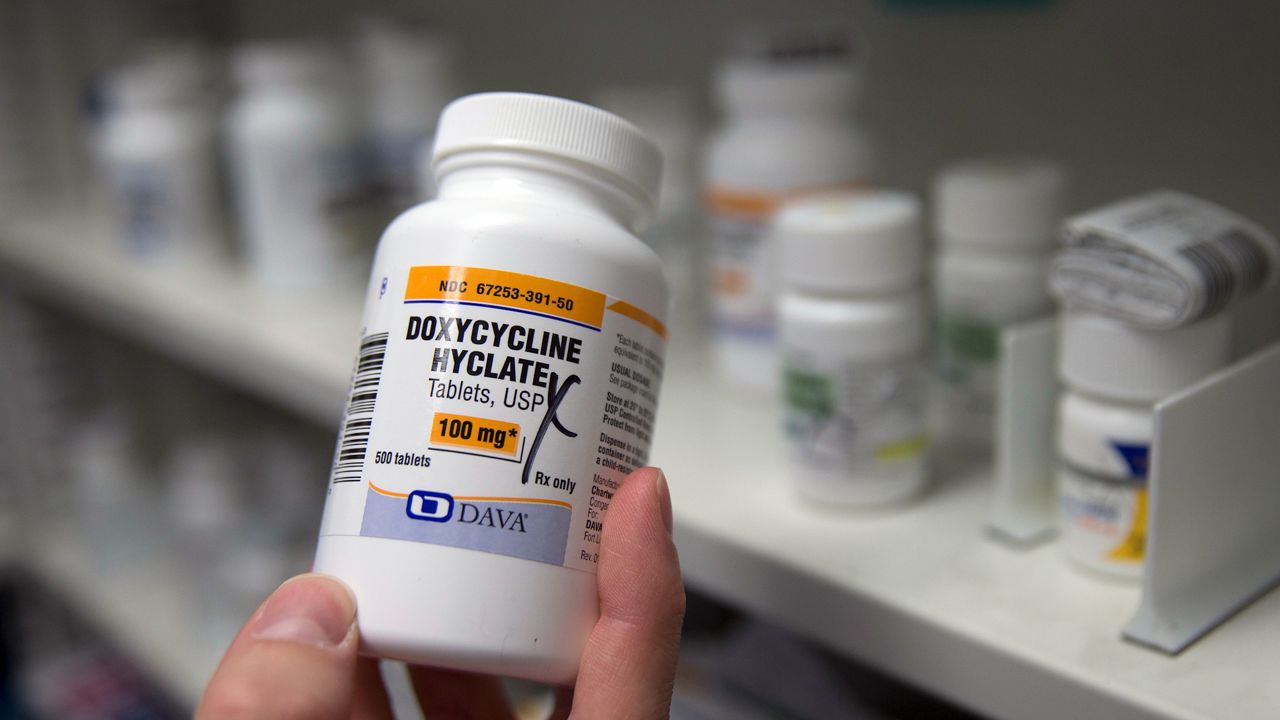
When he first heard about the antibiotic Doxycycline as an option to prevent certain STIs, he thought it was a great idea. The treatment is commonly referred to as DoxyPep. It’s already being used in LA County but is still awaiting final approval from the Centers for Disease Control and Prevention.
“It’s not a replacement for condoms but anything that can help prevent contracting an STI. I think it’s awesome,” Turpin said.
He even took it himself this past summer while on a trip to Europe.
“It was really easy,” he said. “I took it 24 hours after my sexual encounter, and I didn’t have any STIs, which was great!”
Studies show gay and bisexual men as well as transgender women with a previous STI in the past year who took the pills within three days of unprotected sex were about 90% less likely to get chlamydia, had an 80% lower risk of syphilis and over 50% less likely to get gonorrhea. Researchers say the sooner it’s taken, the more effective.
Dr. Kaiyti Duffy is the chief medical officer at the Los Angeles LGBT Center.
“We have precedent for using Doxycycline in a regular basis in acne treatment and prevention and malaria as well,” Duffy said.
She says it’s especially important because there’s a shortage of syphilis medication that could last through early next year.
“The California Department of Public Health has issued support of DoxyPep, so has Los Angeles County. CDC is still gathering information and is likely going to come out in favor,” she said.
The proposed CDC guideline will likely be finalized sometime in November, which could have a big impact since some doctors have been reluctant to talk to patients about it until they heard from the CDC. Dr. Duffy believes the pandemic probably contributed to soaring levels of infections along with a decrease in public funding for STI testing.
“Any time you put a barrier in the way of people accessing care, you’re going to see an uptick in infections and that’s what we’re seeing now,” Duffy said.
Health officials say there’s less evidence the approach works for other people, including heterosexual men and women, but that could change as more research is done. There is also some concern about the overuse of antibiotics.
“We’re not entirely sure about how this is going to impact the gut microbiome. There are also questions about what this will mean for long-term resistance,” Duffy said.
“There are so many faux pas about talking about sex, and I get to do it all day and make it a safe environment for people, and I get to show them that they’re not judged,” Turpin said.
He sees it as one more tool to improve sexual health while fighting the stigma that comes with it.
Let Inside the Issues know your thoughts and watch Monday through Friday at 8 and 11 p.m. on Spectrum News 1.