Cardiovascular
Cardiovascular events and venous thromboembolism after primary malignant or non-malignant brain tumour diagnosis: a population matched cohort study in Wales (United Kingdom)
Participant characteristics
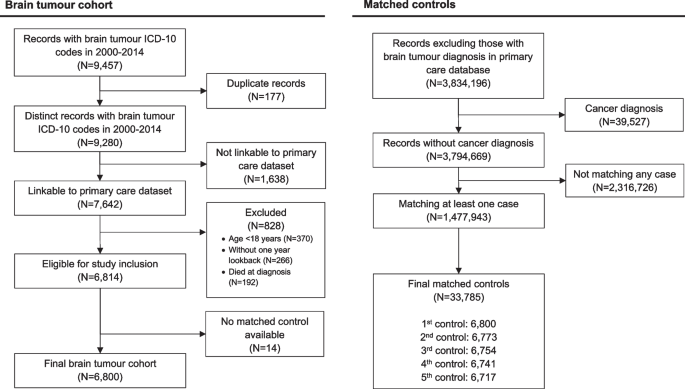
This study included 6800 patients with primary brain tumour diagnosed in Wales 2000–2014 and their 33,785 age-, sex- and GP practice-matched controls. Cohort selection is presented in Fig. 1. The total follow-up time for brain tumour patients and their controls were 32,453.9 person-year (median 3.5 years; interquartile range [IQR] 3.5–10.1) and 247,142.1 person-year (median 6.6 years; IQR 3.9–10.3), respectively. There were 2869 patients with malignant tumour, of which 1340 (46.1%) were glioblastoma. Among 3931 patients with non-malignant tumour, 1498 (38.1%) had non-malignant meningioma. Characteristics of the study cohort are presented in Table 1. Characteristics of matched cohorts for glioblastoma and meningioma are presented in Additional File 1: Table S1. Primary treatment data is available in Additional File 1 Table S2.
Cohort selection for this matched cohort study of people in the SAIL Databank in Wales (UK) 2000–2014. This study included 6800 of 6814 (99.8%) eligible patients diagnosed with a malignant or non-malignant tumour. Of the 1,477,932 eligible controls, 33,765 (2.3%) were included as the matched controls. Controls have no cancer diagnosis and were matched for date of birth within 5 years, sex and GP practice
Malignant tumours
Among 2869 patients with malignant tumours, 252 (8.8%) patients had at least one cardiovascular event within 1 year of diagnosis. There were 89 patients with a major vascular event and 170 patients with VTE (Fig. 2). The crude incidence rates per 1000 person-year in patients with malignant brain tumour and their controls in the first year were 54.1 (95% CI 43.4–66.6) and 48.1 (95% CI 44.5–52.0) for major vascular outcomes and 106.7 (95% CI 91.3–124.0) and 4.9 (95% CI 3.8–6.2) for VTE, respectively. In the fully adjusted Cox models, malignant brain tumour was associated with VTE (hazard ratio [HR] 21.58, 95% CI 16.12–28.88, p < 0.001), haemorrhagic stroke (HR 6.63, 95% CI 3.75–11.70, p < 0.001), and ischaemic stroke (HR 1.88, 95% 95% CI 1.06–3.36, p = 0.032) but not IHD (HR 0.67, 95% CI 0.45–1.00, p = 0.051) or aortic and peripheral vascular disease (HR 1.17, 95% CI 0.56–2.47, p = 0.674). In multivariable analyses of patients surviving 1 year compared to controls, malignant brain tumour diagnosis was associated with VTE (HR 2.20, 95% CI 1.52–3.18, p < 0.001) and all stroke types combined (HR 1.45, 95% CI 1.00–2.10, p = 0.047) (Fig. 2). One-year survivors had lower risk of IHD compared with their controls (HR 0.58, 95% CI 0.37–0.89, p = 0.013).

Crude incidences and hazard ratios for cardiovascular events after tumour diagnosis in people with malignant or non-malignant brain tumour diagnosis compared with their matched controls. Multivariable Cox regression adjusted for brain tumour diagnosis, Welsh index of multiple deprivation, heavy alcohol use, hypercholesterolaemia, past major vascular events, past venous thromboembolism, antiplatelet use, anticoagulant use, antihypertensive use, age and sex
Non-malignant tumours
In 3931 patients with non-malignant tumours, 329 (8.4%) patients had at least one cardiovascular event within 1 year of diagnosis. There were 265 patients with a major vascular event and 96 patients with VTE (Fig. 2). The incidence rates per 1000 person-year in patients with non-malignant tumour, and their controls in the first year were 78.8 (95% CI 69.6–88.8) and 40.3 (95% CI 37.5–43.3) for major vascular outcomes and 20.0 (95% CI 15.5–25.3) and 5.4 (95% CI 4.4–6.5) for VTE, respectively. In the multivariable analysis, a non-malignant tumour diagnosis was associated with VTE (HR 3.72, 95% CI 2.73–5.06, p < 0.001), haemorrhagic stroke (HR 4.18, 95% CI 2.59–6.74, p < 0.001), ischaemic stroke (HR 3.52, 95% CI 2.69–4.61, p < 0.001) and aortic and peripheral arterial disease (HR 2.09, 95% CI 1.26–3.48, p = 0.003). In those surviving 1 year after tumour diagnosis, non-malignant tumour compared to controls was associated with a lower risk of haemorrhagic stroke (HR 0.55, 95% CI 0.37–0.83, p = 0.004), ischaemic heart disease (HR 0.65, 95% CI 0.56–0.76, p < 0.001) and aortic and peripheral arterial disease (HR 0.60, 95% CI 0.44–0.84, p = 0.003) (Fig. 2).
Tumour subgroups
There were 1340 patients with glioblastoma (Additional File 1: Table S1), and 137 (10.2%) of these patients had at least one cardiovascular event within 1 year of diagnosis. Thirty-six (2.7%) patients had a major vascular event, and 107 (8.0%) patients had VTE (Additional File 1: Figure S2). The incidence rates per 1000 person-year in glioblastoma patients and their controls in the first year were 50.7 (95% CI 35.5–70.3) and 52.6 (95% CI 47.1–58.6) for major vascular outcomes and 159.4 (95% CI 130.6–192.6) and 4.7 (95% CI 3.2–6.8) for VTE, respectively. In the adjusted Cox models, glioblastoma diagnosis was associated with VTE (HR 31.78, 95% CI 20.99–48.13, p < 0.001) and haemorrhagic stroke (HR 5.02, 95% CI 2.16–11.67, p < 0.001) (Additional File 1: Figure S2). We did not examine these associations in patients surviving 1 year because of the small number of outcomes observed. There were 291 patients with glioblastoma surviving 1 year without a cardiovascular event, of which 15 developed a CVD during the remaining follow-up time.
Of the 1498 patients with meningioma (Additional File 1: Table S1), 184 (12.3%) had at least one cardiovascular event within 1 year of diagnosis. Major vascular event and VTE occurred in 162 (10.8%) and 36 (2.4%) patients, respectively. The incidence rates per 1000 person-year in meningioma patients and their controls were 123.6 (95% CI 104.7–145.0) and 52.0 (95% CI 46.8–57.7) for major vascular events and 29.6 (95% CI 20.9–40.6) and 4.9 (95% CI 3.4–6.8), respectively. In multivariable models, meningioma diagnosis was associated with VTE (HR 5.90, 95% CI 3.71–9.38, p < 0.001), haemorrhagic stroke (HR 3.80, 95% CI 2.01–7.18, p < 0.001) and ischaemic stroke (HR 4.37, 95% CI 3.09–6.18, p < 0.001). Patients with meningiomas alive 1 year after tumour diagnosis had lower risk of haemorrhagic stroke (HR 0.37, 95% CI 0.17–0.80, p = 0.011), ischaemic heart disease (HR 0.72, 95% CI 0.55–0.93, p = 0.013), and aortic and peripheral arterial disease (HR 0.45, 95% CI 0.23–0.86, p = 0.015) (Additional File 1: Figure S2).
Incidence of cardiovascular events during first year of diagnosis
Using multivariable flexible parametric models, we estimated the incidence of major vascular events and VTE for tumour groups stratified by age (Fig. 3). The incidence of VTE showed a bimodal distribution with peaks at 1 month and 5 months in malignant tumours. People with non-malignant tumours had the highest incidence of major vascular events early after tumour diagnosis. Patients who underwent surgery for malignant brain tumour had highest risks of VTE at 1 and 5 months after diagnosis, but this was not observed in those not receiving surgery (Additional File 1: Figure S3). Incidence trends of outcome events in patients with malignant tumour stratified by surgery status was similar to the overall trends.

Incidences of major vascular and venous thromboembolic events within 1 year of study entry. We used flexible parametric survival models with four degrees of freedom adjusted for brain tumour diagnosis, Welsh index of multiple deprivation, heavy alcohol use, hypercholesterolaemia, past major vascular events, past venous thromboembolism, antiplatelet use, anticoagulant use, antihypertensive use, age and sex to estimate CVD incidences. Predicted incidences at ages 50, 65 and 75 years were generated
Sensitivity analyses
Analyses using multivariable Cox models, including BMI and smoking status, showed similar results to the main analyses (Additional File 1: Figure S4). Because a high proportion of stroke occurred shortly after tumour diagnosis, we removed brain tumour patients having a stroke within 14 days. In patients with malignant tumours surviving 14 days without a stroke, they had higher risks of all stroke types combined (including unspecified stroke) and haemorrhagic stroke (Additional File 1: Figure S5). In patients with non-malignant tumours surviving 14 days without a stroke, they had higher risk of all stroke subtypes (Additional File 1: Figure S6). The direction of subhazard ratios in the competing risk analyses were consistent with cause-specific analyses presented in Figs. 2 and 3 (Additional File 1: Table S3 and S4).
Use of antiplatelet and cardiovascular outcomes
The absolute numbers of patients suffered cardiovascular outcomes within first year of diagnosis by tumour type, surgery status and use of antiplatelet are presented in Table 2. Some numbers are not presented due to data suppression to minimise disclosure risk. Across patient groups, the proportions of patients who had major vascular events were higher in those on an antiplatelet drug at the time of diagnosis, except for patients with meningioma who did not have surgery.