Infection
Why does COVID-19 cause brain fog? Scientists may finally have an answer.
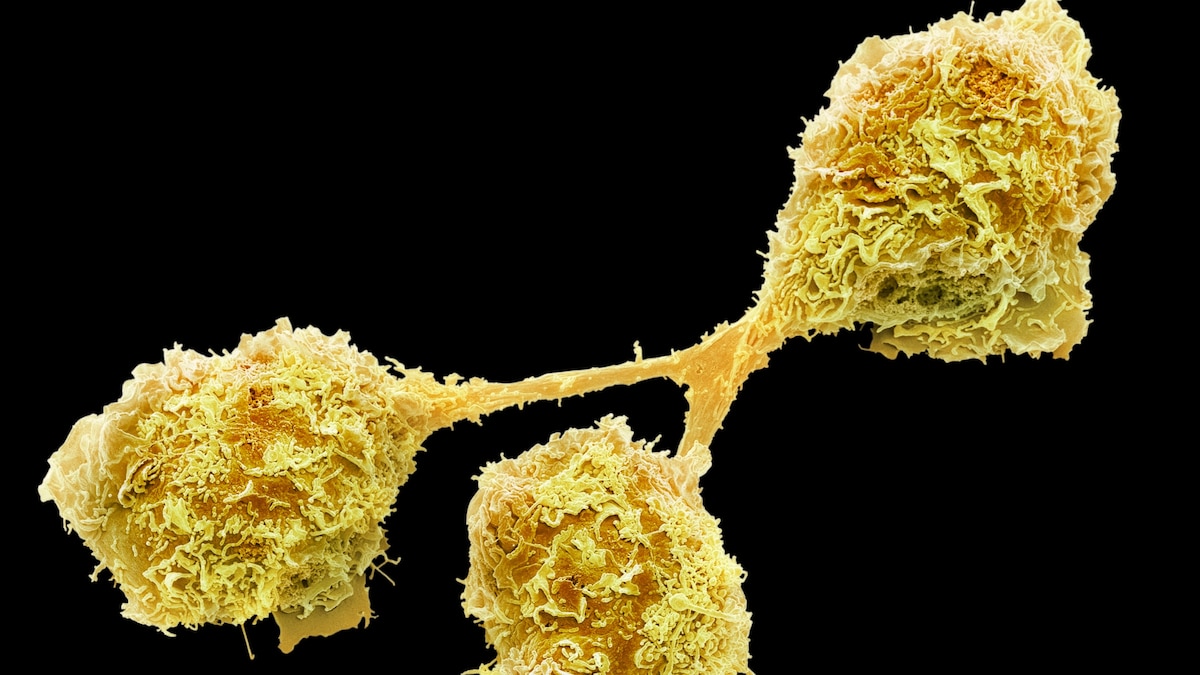
When scientists infected brain organoids—pinhead-size bits of brain tissue grown in the lab—with the virus that causes COVID, they found that not only does it spread in neurons in the brain, it also accelerates the destruction of connections between neurons—called synapses—that are essential for communication.
These discoveries expand understanding of how SARS-CoV-2 can damage the nervous system. COVID-19 patients continue to suffer with a range of symptoms, especially neural and behavioral problems, long after the infection. One such condition, commonly known as brain fog, causes disorientation, memory loss, chronic headache, and numbness, and it affects nearly 40 percent of long COVID patients.
“There are many case reports, even some in our own clinic, of patients who have symptoms [of brain fog] lasting upwards of a year,” says Ayush Batra, a neurologist at Northwestern University Feinberg School of Medicine.
Carl Sellgren, a psychiatrist and cellular biologist, and his team at the Karolinska Institute in Sweden used organoids to study what SARS-CoV-2 does to brain.
“It was quite striking that very small amounts of the virus could quite rapidly spread in the organoids and eliminate an excessive number of synapses,” says Ana Osório Oliveira, a neuroscientist in Sellgren’s team.
Another study found that spike protein—which coats the outer surface of the virus—directly eliminates synapses causing loss of memory in lab mice by causing inflammation.
Destroying too many connections between neurons, or over-pruning, may be causing brain fog in long COVID patients. “This could be one of the many reasons—probably—why we are observing a range of neurological symptoms, even after the infection is long gone,” says Samudyata, a postdoctoral researcher at Karolinska Institute who led the study and only uses one name.
Virus has been found in autopsied brain tissues and throughout the bodies of patients, who died more than 200 days after contracting COVID-19. It is evidence that the virus is capable of persisting in organs throughout the body.
“There are some persistent virus reservoirs that can cause a chronic inflammatory response or autoimmune attack on the brain, which can cause pruning and brain shrinkage,” says Batra.
Pruning connections between neurons is essential for learning
The brain is made of a dense and dynamic network of nerve cells that communicate through synapses that change as humans learn. “Synapses are essentially how cells talk to each other and how information is passed from one part of the brain to another,” Lancaster says.
Synapses are responsible for all the functions of the brain, from memory to controlling movement to feeling emotions, and they are constantly remodeled. “That’s how we learn,” she says.
The junctions between neurons that talk to each other frequently have more knob-shaped synapses that produce neurotransmitters—chemicals that transmit signals to other neurons. Conversely, neurons that communicate less or not at all have fewer synapses because they are removed, or pruned, by immune cells called microglia. Microglia make up to 17 percent of the cell population in some parts of the human brain and perform housekeeping duties by migrating through the brain eating dead cells and scavenging weak synapses.
Although synaptic pruning is most active in developing brains such as in fetuses and infants, it continues in healthy brains throughout life and is necessary for encoding new memories and erasing the ones it no longer needs. Synaptic pruning is also critical for the brain to recover from an injury; allowing it to strengthen synapses which relearn the lost skills and remove synapses that no longer function.
Using brain organoids to study neural damage
Studying a direct link between COVID-19 and cognitive dysfunction, such as brain fog, is difficult in living brains. That is why studies are often limited to cadavers of COVID-19 patients. But brain organoids, often called mini-brains, allow scientists to see in real time how SARS-CoV-2 affects living tissue.
Mini-brains can be used to study infection because scientists can control the amount of viruses that are exposed to individual cells, says Oliver Harschnitz, group leader in the Neurogenomics Research Centre at Human Technopole Institute in Milan, Italy, even though tissue organization is less structured than real brains.
Using brain organoids, Oliveira and her colleagues found that the virus itself was not directly pruning the synaptic connections but was activating the microglia.
“We found that following infection by SARS-CoV-2, somehow the microglia become immunoreactive, and eat more of the synapses than normal,” Samudyata says.
It’s a very interesting study because it really shows the quantitative differences in the microglial activity after COVID-19 and its effect on synapses says Ayush Batra, a neurologist at Northwestern University Feinberg School of Medicine.
Too much synapse pruning can be detrimental and has been linked to neurodevelopmental disorders such as schizophrenia, as well as neurodegenerative disorders such as Alzheimer’s and Parkinson’s diseases.
In a follow-up study, Sellgren’s team has found that a protein called C4A—which helps remove microbes and infected cells—also tags synapses for removal. Although his research doesn’t directly connect C4A with brain fog, it suggests that inflammation after infection can affect pruning of synapse, depending on genetics, says Sellgren.
If the excessive elimination of synapses that occur in brain organoids after SARS-CoV-2 infection also occurs in people, it may destroy vital connections and explain why some with COVID-19 suffer from long-term neurological symptoms.
“Too much synapse elimination would be expected to affect a person’s ability to form new memories, or to remember existing ones, and could help explain the sluggish brain functions seen in brain fog,” Lancaster says.
This is consistent with studies done at the U.S. National Institutes of Health that have found antibodies produced in response to SARS-CoV-2 can attack the cells lining the brain’s blood vessels, causing damage and inflammation—which activates microglia—even if the virus doesn’t directly enter the brain. That may explain why, as Batra’s team has shown, some long COVID patients not sick enough to be hospitalized continue to experience neurologic symptoms beyond a year after initial infection.
Is the loss of synapses causing brain shrinkage?
A U.K. study has also shown that even mild COVID-19 can shrink the brain through loss of gray matter—the outermost layer of the brain that is vital for controlling movement, memory, and emotions—causing physical changes equivalent to a decade of aging. A new study, which has not yet been peer-reviewed, suggests that COVID-19 can accelerate the decline of cognitive ability equivalent to ten years of normal aging, especially after severe COVID disease or severe long COVID.
“We are still unclear what may contribute, in general, to a loss of gray matter volume or thickness observed using MRI,” says Gwenaëlle Douaud, a neuroscientist at the University of Oxford who led the study.
While synapse elimination, as shown in Samudyata’s study, could account for a small percentage of the change in the gray matter, says Douaud, more studies combining imaging with tissue sections are required to determine the other factors that lead to brain shrinkage.
Hyperactive microglia may cause problems in other ways. The Swedish study also shows that the pattern of genes turned on and off by the microglia in brain organoids after SARS-CoV-2 infection mimicked gene activity seen in neurodegenerative disorders. This may explain why there is a three times higher risk of developing neurological or psychiatric conditions within six months after COVID-19 compared with those who were not infected. In adults aged over 65, the risk of developing dementia after a COVID-19 infection is almost twice that of other respiratory infections.
However, scientists caution that much more research is needed to understand the effect of SARS-CoV-2 infection on the brain. As organoids resemble immature cells—like those in a fetal or post-natal state—this limits extrapolation of the results to mature adult brain cells.
“While these data are exciting and indicate a role for proinflammatory microglia in the disease mechanisms underlying long COVID, more studies are required to validate these findings and build on them,” Harschnitz says.
It’s also not known how long COVID affects quality of health and whether it has long term or irreversible effects on the brain. So as the pace of holiday and indoor winter activities picks up, Samudyata advises taking preventative measures and staying up to date on vaccinations to minimize the chance of getting COVID over and over. While it isn’t clear how the virus exerts detrimental effects on the brain, it’s evident that it does cause damage.
Editor’s note: This story was originally published on December 2, 2022. It has been updated to include the latest research.