Congenital disorders
Low Back Pain in resident doctors
Introduction
Low back pain (LBP) is a highly prevalent and disabling health condition, affecting people of all ages worldwide.1 It is the leading cause of global disability and results in enormous economic and social burdens.2 In the general population, the 1-year prevalence of LBP ranges from 22% to 65%, with a lifetime prevalence exceeding 84% in some studies.3 Healthcare workers, especially physicians, are at high risk for developing LBP due to occupational exposures such as prolonged standing, frequent bending and twisting, lifting and transferring patients, high psychological demands, and lack of control over work.4,5 In China, a national survey of over 20,000 physicians found a 1-year LBP prevalence of 65.5%.6
Resident physicians are particularly vulnerable to LBP and work-related musculoskeletal disorders due to their intensive training requirements on top of provision of patient care.7 The typical duties of residency training involve overwork, sleep deprivation, rotational night shifts, and enduring awkward postures during patient care and procedures.8–10 Studies from countries with established residency programs have revealed a high prevalence of LBP among resident physicians. For instance, a study in a Tertiary Level Hospital of Bangladesh reported a 68.6% prevalence of LBP.11
In China, concerns over the competency of residency training have led policymakers to initiate a nationwide standardized residency training program since 2015.12 The standardized model aims to improve clinical skills and professionalism through rigorous didactic teaching and rotations.13
However, the intense workload and training requirements may put medical worker at increased risk for LBP.14 While a few studies have examined LBP among Chinese resident physicians prior to the initiation of standardized training, research specifically evaluating LBP prevalence and related factors in residents with standardized training remains scarce.6,15 Resident doctors are in a critical stage of their career development, where they face intense workload, long working hours, and high expectations from supervisors and patients. These factors may increase their susceptibility and vulnerability to LBP. Given the high prevalence and substantial disability caused by LBP in resident doctors, further research is needed to elucidate the magnitude of this problem and identify associated factors to guide preventive strategies in this population undergoing intensive standardized training.16 Therefore, it is important to investigate the prevalence and impact of LBP among resident doctors and identify the associated factors that can be modified or prevented. Therefore, the aim of this study was to investigate the prevalence and impact of LBP in resident doctors with standardized training in a tertiary hospital in China. The findings of this study may provide useful information for developing effective interventions to prevent and manage LBP among resident doctors.
Methods
Study Design
This cross-sectional study aimed to investigate the prevalence and risk factors of LBP in doctors with standardized training in China.
Study Setting and Participants
The participants were doctors who had completed or were undergoing standardized training in 3 hospitals in Sichuan Province, China. Standardized training is a national program that requires doctors to complete three years of postgraduate training in a designated specialty after graduating from medical school. The inclusion criteria were: (1) being a doctor with standardized training for more than 1 year; (2) being aged between 25 and 45 years; (3) being willing to participate in the study. The exclusion criteria were: (1) having a history of spinal surgery or trauma; (2) having a diagnosis of inflammatory or infectious spinal diseases, spinal tumors, or congenital spinal anomalies; (3) being pregnant or lactating.
Procedures
The study was approved by the ethics committee of the Affiliated Hospital of North Sichuan Medical College and conducted between January and June 2023, and this study was conducted in accordance with the Declaration of Helsinki. The participants were recruited by convenience sampling from 3 hospitals. They were informed about the purpose and procedures of the study and gave written informed consent. They were asked to complete a self-administered questionnaire that collected demographic data, occupational data, and information on LBP. The questionnaire was based on the standardized Nordic questionnaire for musculoskeletal symptoms and modified according to the Chinese context. The sample size was calculated based on the expected prevalence of LBP among doctors with standardized training, which was estimated to be 72.8% based on previous studies.17 Assuming a confidence level of 95%, a margin of error of 5%, according to the formula (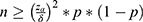 ), the minimum sample size is 305. To account for possible non-response or incomplete data, we increased the sample size by 20%, resulting in a final sample size of 382. And our questionnaire response rate was 90.31% (345).
), the minimum sample size is 305. To account for possible non-response or incomplete data, we increased the sample size by 20%, resulting in a final sample size of 382. And our questionnaire response rate was 90.31% (345).
Measures
LBP was defined as pain or discomfort in the area between the lower margin of the 12th rib and the lower gluteal folds, with or without leg pain, lasting for at least one day in the past 12 months.3 The participants were asked to report the intensity and impact of LBP on their daily activities and work performance. The intensity of LBP was measured by a 10-point numerical rating scale, where 0 indicated no pain and 10 indicated the worst pain imaginable. The impact of LBP on daily activities and work performance was assessed by two questions: “How much did LBP interfere with your daily activities in the past 12 months?” and “How much did LBP affect your work performance in the past 12 months?” The answers were rated on a 5-point Likert scale, where 1 indicated not at all and 5 indicated extremely.
The potential risk factors of LBP were divided into individual factors and occupational factors. The individual factors included age (years), gender (male/female), height (cm), weight (kg), body mass index (BMI) (kg/m2), current smoker (yes/no), and regular physical activity (yes/no). Smoking status was defined as smoking in the past 30 days before the data collection.18 Physical activity was defined as exercising for at least 30 minutes or walking for 3 or more days per week.19 The occupational factors included specialty, educational level, and working hours per week (hours). The ergonomic factors included prolonged standing (yes/no), frequent bending or twisting (yes/no), lifting heavy objects (yes/no), and sustained sitting (yes/no), which were based on self-report. These factors have been identified as common ergonomic risk factors for LBP among healthcare workers.20
Data Collection
Data collection was conducted by trained researchers. With the help of the head of the doctor training management department, we distributed the questionnaire to doctors with standardized training. The questionnaires were anonymous and confidential, and the doctors with standardized training were informed about the purpose and procedures of the study. The doctors with standardized training were asked to fill out the questionnaires voluntarily and return them to the researchers within one week.
Data Analysis
The data were analyzed using SPSS software version 25.0. Descriptive statistics were used to summarize the demographic characteristics, lifestyle habits, work-related factors, and LBP-related information of the participants. The prevalence of LBP in the past year was calculated as the percentage of participants who reported having LBP in the past year out of the total number of participants. The mean and standard deviation (SD) were used to describe the pain intensity and the impact scores of LBP on daily life and work. The chi-square test was used to compare the categorical variables between the participants with LBP and those without LBP. The Spearman’s rank correlation coefficient was used to measure the correlation between LBP and continuous variables. A logistic regression model was used to identify the factors associated with LBP among resident doctors with standardized training. The dependent variable was LBP (yes/no), and the independent variables were those that showed a significant difference or correlation with LBP in the univariate analysis. The odds ratio (OR) and 95% confidence interval (CI) were calculated to estimate the strength of association between each factor and LBP. A p-value < 0.05 was considered statistically significant.
Results
General Characteristics
A total of 345 resident doctors participated in this study, with a response rate of 90.31%. The general characteristics of the participants are shown in Table 1. The mean age was 28.64 ± 1.77 years, and 65.8% were female. Among them, 262 (75.9%) reported having LBP in the past year, with a mean pain score of 3.41 ± 2.76 and a mean impact score on life and work of 2.53 ± 1.44 and 2.51 ± 1.39, respectively.
|
Table 1 General Characteristics of the Doctor with Standardized Training |
Univariate Analysis of Factors Related to LBP
The univariate analysis of factors related to LBP is shown in Table 2. There were significant associations between LBP and gender, smoking, physical exercise, working hours per week, frequent bending or twisting, and sustained sitting.
|
Table 2 Univariate Analysis of Factors Related to LBP |
Multivariable Logistic Regression Analysis
The multivariable logistic regression analysis of LBP and its related factors are shown in Table 3. The results indicated that physical exercise, weekly working hours, and sustained sitting were significant predictors of LBP (p <0 0.05). The odds of having LBP were 82.6% lower for those who exercised than those who did not (OR = 0.174, 95% CI: 0.073–0.414). The odds of having LBP were 15.2 times higher for those who worked more than 40 hours per week than those who worked less (OR = 15.236, 95% CI: 2.83–82.018). The odds of having LBP were 13.1 times higher for those who sat for a long time than those who did not (OR = 13.14, 95% CI: 2.423–71.253).
 |
Table 3 Multivariable Logistic Regression Analysis of LBP and Its Related Factors |
Discussion
In this cross-sectional study, we aimed to investigate the prevalence and risk factors of LBP in doctors with standardized training in China. The main findings were that LBP was highly prevalent (75.9%) among resident doctors, and that physical exercise, working hours per week, and sustained sitting were significant predictors of LBP.
Resident doctors with standardized training in China are required to complete a three-year program that involves rotating through different departments, working long hours, and performing various clinical tasks. These factors may increase their exposure to physical and psychological stressors that can contribute to LBP. The prevalence of LBP in our study was lower than that reported in previous studies among nurses (78%)21 in China and medical students (94%) in Saudi Arabia, but higher than healthcare professionals in China (72.8%)17 and in Northwest Ethiopia (57.46%).22 In fact, although there are many peer-reviewed studies on the prevalence or incidence of LBP, there is little agreement on its epidemiology and its risk factors.23–25 This may be due to the differences in the definition and measurement of LBP, the characteristics of the study population, and the work environment and culture of doctors in different regions. Moreover, our study focused on resident doctors who had completed or were undergoing standardized training for more than 1 year, which may represent a specific subgroup of doctors who are exposed to intensive training demands and stressors that may affect their spinal health. However, our finding was consistent with the general trend that LBP is a common occupational health problem among health care workers worldwide.17
The intensive demands of residency training likely contribute to the pronounced burden of LBP in this population. China’s transition to standardized residency programs in 2015 markedly increased training intensity, with most residents now working over 40 hours per week. Our finding that working >40 hours was independently associated with higher LBP risk aligns with past research showing long work hours can increase the risk of musculoskeletal disorders and that having regular working hours can be a protective factor.26 The recurring need for overnight shifts and extended duty hours may prevent adequate rest and recovery, increasing residents’ vulnerability to LBP.4 Weekly working hours can affect the risk and severity of LBP by influencing the physical and psychological well-being of the individual.27 Long working hours can lead to fatigue, reduced recovery time, and increased exposure to physical and psychosocial demands. Long working hours can also interfere with the work-life balance and affect the quality of sleep, which are important for maintaining health and well-being.28,29 However, our study also found that 71% of the resident doctors with standardized training in China worked more than 40 hours per week. This may be due to the high demand and expectation for resident doctors to complete their training program and pass their examinations. Therefore, interventions to reduce working hours and improve working conditions among resident doctors with standardized training in China are needed.
Sustained sitting was found to be a risk factor for LBP in our study, which is supported by the previous studies.30,31 Sustained sitting can compromise metabolic health32 and decreased muscle strength, force control and ability to maintain balance.33 Sustained sitting can cause biomechanical changes in the spine, such as reduced disc height, increased disc pressure, and decreased blood flow, which can lead to disc degeneration and inflammation.34–37 Sustained sitting can also result in poor posture, muscle imbalance, and reduced spinal mobility.38,39 However, our study also found that 77.7% of the resident doctors with standardized training in China sat for a long time. This may be due to the nature and requirement of their work, such as writing reports, reading articles, attending lectures, and performing procedures. Therefore, strategies to reduce sitting time, such as standing or walking breaks, ergonomic optimizations, and promotion of incidental physical activity should be considered for resident doctors.40,41
Physical exercise was found to be a protective factor for LBP in our study, which is consistent with the current evidence and guidelines.42–44 This aligns with existing evidence that exercise strengthens core muscles, preventing deconditioning and spine dysfunction.40,45 Physical exercise can reduce the risk and severity of LBP by improving the physical and mental health of the individual.46 Physical exercise can enhance the musculoskeletal health of the spine and modulate the pain perception in the central nervous system.47 Physical exercise can also have positive effects on mental health, such as reducing stress,48 anxiety and depression,49 which are known to be associated with LBP.50,51 However, our study also found that only 21.2% of the resident doctors with standardized training in China engaged in physical exercise. This may be due to the lack of time, motivation, facilities, and support for physical activity among this population. Therefore, interventions to promote physical activity among resident doctors with standardized training in China are needed.
Interestingly, some established LBP risk factors like high BMI and heavy lifting did not emerge as significant in our study, despite prior evidence linking obesity and manual handling to increased spine loading.52,53 Additionally, prolonged standing was not a significant LBP predictor, contrasting with other studies showing static standing elevates risk.54 These discordances warrant further investigation but may reflect underlying differences in body composition, clinical duties, and workplace ergonomics between Chinese and Western populations. Another possibility is that, due to the occupational of resident doctors with standardized training, traditional indicators such as BMI, heavy lifting and prolonged standing are not that important. Although BMI is used as a parameter of obesity, it cannot represent the percentage and distribution of body fat.55 New imaging indicators such as the subcutaneous fat index (SFI) and subcutaneous fat tissue thickness (SFTT) were superior to BMI in predicting LBP and spine degeneration.55,56 Therefore, we believe that with the improvement of examination methods, some new examination indicators may be more suitable for assessing LBP risk factors and can be provided to employees during the physical examination of resident physicians, instead of BMI or other traditional indicators.
Furthermore, our study also has some limitations. 1st, our study was cross-sectional, which mainly focused on the epidemiological aspects of LBP and limited the causal inference between LBP and its risk factors. To explore the clinical aspects and impact of LBP on resident doctors, some possible instruments and methods for assessing these aspects, such as the Oswestry Disability Index, the Roland-Morris Disability Questionnaire, and the visual analog scale are required. Longitudinal studies are needed to establish the temporal relationship and directionality of these associations. 2nd, our study relied on self-reported data, which may be subject to recall bias and social desirability bias. 3rd, some factors that have been reported to be related to LBP in previous studies, such as psychosocial factors,57 ergonomic factors,58 and genetic factors,59 were not assessed in our study. Finally, we also recognize that our sample may not be fully representative of the whole population of resident doctors in China, as there may be regional and institutional variations in the characteristics and experiences of resident doctors. Therefore, further studies with larger sample sizes, more comprehensive measurements, and more advanced statistical methods are needed to confirm or refute our findings. Future studies should consider these factors in their analyses.
In conclusion, our study showed that LBP was a common problem among resident doctors with standardized training in China. Physical exercise, weekly working hours, and sustained sitting were significant predictors of LBP. These findings suggest that we may need new indicators instead of traditional BMI, lifting and prolonged standing interventions to predict the risk of low back pain, and interventions to prevent and manage LBP among resident doctors with standardized training should focus on promoting physical activity, reducing working hours, and improving sitting posture. Further research is needed to confirm these findings and to evaluate the effectiveness of these interventions.
Acknowledgment
The study was carried out with the support of a grant (2022LC017) from Affiliated Hospital of North Sichuan Medical College. We would like to thank all the resident doctors with standardized training who participated in this study for their time and cooperation. We would also like to thank the hospital administrators and managers for their support and facilitation of the data collection. We would like to express our sincere gratitude to Han-Wen Zhang and Hong-Ping Tan, who contributed equally to this work as co-first authors. They were involved in the conception, design and ethical approval for the study, as well as in the drafting and revising of the manuscript. We would also like to thank Qiu-Xia Feng for their assistance in data collection, analysis and interpretation of the data. All authors have read and approved the final manuscript.
Funding
The study was carried out with the support of a grant (2022LC017) from Affiliated Hospital of North Sichuan Medical College.
Disclosure
Han-Wen Zhang and Hong-Ping Tan are co-first authors for this study. The authors report no conflicts of interest in this work.
References
1. Buchbinder R, Van Tulder M, Öberg B, et al. Low back pain: a call for action. Lancet. 2018;391(10137):2384–2388. doi:10.1016/S0140-6736(18)30488-4
2. James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858 doi:10.1016/s0140-6736(18)32279-7.
3. Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–2037. doi:10.1002/art.34347
4. Wong T, Teo N, Kyaw M. Prevalence and risk factors associated with low back among health care providers in a district hospital. Malays Orthop J. 2010;4(2):23–28. doi:10.5704/MOJ.1007.004
5. Alghadir A, Zafar H, Iqbal ZA, et al. Work-related low back pain among physical therapists in Riyadh, Saudi Arabia. Workplace Health Saf. 2017;65(8):337–345. doi:10.1177/2165079916670167
6. Yang H, Haldeman S, Lu M-L, et al. Low back pain prevalence and related workplace psychosocial risk factors: a study using data from the 2010 national health interview survey. J Manipulative Physiol Ther. 2016;39(7):459–472. doi:10.1016/j.jmpt.2016.07.004
7. Bos E, Krol B, Van Der Star L, et al. Risk factors and musculoskeletal complaints in non-specialized nurses, IC nurses, operation room nurses, and X-ray technologists. Int Arch Occup Environ Health. 2007;80:198–206. doi:10.1007/s00420-006-0121-8
8. Meric R, Stone RG, Lupu VV, et al. The diversity of pediatric residency programs across Europe: quality assurance of training, night shifts, and wages. J Pediatr. 2020;226:319–320.e2. doi:10.1016/j.jpeds.2020.08.001
9. Ishikawa M. Overwork among resident physicians: national questionnaire survey results. BMC Med Educ. 2022;22(1):729. doi:10.1186/s12909-022-03789-7
10. Xu Y, Chen G, Han X, et al. Overwork death of Chinese physicians under high-intensity pressure, 2007–2018. Iran J Public Health. 2020;49(12):2251–2255. doi:10.18502/ijph.v49i12.4804
11. Rahman MA, Khan MA, Akter MR, et al. Proportion of low back pain among physicians working in a tertiary level hospital of Bangladesh. Mymensingh Med J. 2021;30(2):262–266.
12. Chen Q, Li M, Wu N, et al. A survey of resident physicians’ perceptions of competency-based education in standardized resident training in China: a preliminary study. BMC Med Educ. 2022;22(1):801. doi:10.1186/s12909-022-03863-0
13. National Health and Family Planning Commission General Office. Notice from the general office of the national health and family planning commission on issuing the implementation measures for the standardized training and recruitment of resident physicians (Trial Implementation) and the implementation measures for the standardized training and assessment of resident physicians (Trial Implementation)”; 2015. Available from: http://www.nhc.gov.cn/qjjys/s3593/201510/e9edb9ed82224b28bc935188f9f1ff38.shtml. Accessed August 30, 2023.
14. Shieh SH, Sung FC, Su CH, et al. Increased low back pain risk in nurses with high workload for patient care: a questionnaire survey. Taiwan J Obstet Gynecol. 2016;55(4):525–529. doi:10.1016/j.tjog.2016.06.013
15. Lin Y-H, Chen C-Y, S-Y L. Physical discomfort and psychosocial job stress among male and female operators at telecommunication call centers in Taiwan. Appl Ergon. 2009;40(4):561–568. doi:10.1016/j.apergo.2008.02.024
16. Trinkoff AM, Storr CL, Lipscomb JA. Physically demanding work and inadequate sleep, pain medication use, and absenteeism in registered nurses. J Occup Environ Med. 2001;43:355–363. doi:10.1097/00043764-200104000-00012
17. Dong H, Zhang Q, Liu G, et al. Prevalence and associated factors of musculoskeletal disorders among Chinese healthcare professionals working in tertiary hospitals: a cross-sectional study. BMC Musculoskelet Disord. 2019;20(1):175. doi:10.1186/s12891-019-2557-5
18. Jamal A, King BA, Neff LJ, et al. Current cigarette smoking among adults – United States, 2005–2015. MMWR Morb Mortal Wkly Rep. 2016;65(44):1205–1211. doi:10.15585/mmwr.mm6544a2
19. World Health Organization GWH. WHO Guidelines Approved by the Guidelines Review Committee. In: Global Recommendations on Physical Activity for Health. Geneva, Switzerland: World Health Organization; 2010.
20. Da Costa BR, Vieira ER. Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am J Ind Med. 2010;53(3):285–323. doi:10.1002/ajim.20750
21. Wang D-Y, Sun -Y-Y. Prevalence and influencing factors of low back pain among nurses in China: a systematic review and meta-analysis. Frontiers of Nursing. 2021;7(4):329–336. doi:10.2478/fon-2020-0042
22. Negash NA, Tadele A, Jember Ferede A. Prevalence and associated factors of low back pain among healthcare professionals at University of Gondar comprehensive and specialized hospital, northwest Ethiopia: cross-sectional study. J Pain Res. 2022;15:1543–1552. doi:10.2147/JPR.S351987
23. Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–939. doi:10.1016/j.jclinepi.2011.11.014
24. Hoy D, Brooks P, Blyth F, et al. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769–781. doi:10.1016/j.berh.2010.10.002
25. Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord. 2000;13(3):205–217 doi:10.1097/00002517-200006000-00003.
26. Nabi MH, Kongtip P, Woskie S, et al. Factors associated with musculoskeletal disorders among female readymade garment workers in Bangladesh: a comparative study between OSH compliant and non-compliant factories. Risk Manag Healthc Policy. 2021;Volume 14:1119–1127. doi:10.2147/RMHP.S297228
27. Wami SD, Abere G, Dessie A, et al. Work-related risk factors and the prevalence of low back pain among low wage workers: results from a cross-sectional study. BMC Public Health. 2019;19(1):1–9. doi:10.1186/s12889-019-7430-9
28. Waddell G. Occupational health guidelines for the management of low back pain at work: evidence review. Occup Med. 2001;51(2):124–135. doi:10.1093/occmed/51.2.124
29. Bernstein IA, Malik Q, Carville S, et al. Low back pain and sciatica: summary of NICE guidance. BMJ. 2017;356:i6748 doi:10.1136/bmj.i6748.
30. Baradaran Mahdavi S, Riahi R, Vahdatpour B, et al. Association between sedentary behavior and low back pain; A systematic review and meta-analysis. Health Promot Perspect. 2021;11(4):393–410. doi:10.34172/hpp.2021.50
31. Barone Gibbs B, Hergenroeder AL, Perdomo SJ, et al. Reducing sedentary behaviour to decrease chronic low back pain: the stand back randomised trial. Occup Environ Med. 2018;75(5):321–327. doi:10.1136/oemed-2017-104732
32. Owen N, Healy GN, Matthews CE, et al. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38(3):105–113. doi:10.1097/JES.0b013e3181e373a2
33. Mear E, Gladwell VF, Pethick J. The effect of breaking up sedentary time with calisthenics on neuromuscular function: a preliminary study. Int J Environ Res Public Health. 2022;19(21):14597. doi:10.3390/ijerph192114597
34. Salo S, Hurri H, Rikkonen T, et al. Association between severe lumbar disc degeneration and self-reported occupational physical loading. J Occup Health. 2022;64(1):e12316. doi:10.1002/1348-9585.12316
35. You Y, Chen Y, Fang W, et al. The association between sedentary behavior, exercise, and sleep disturbance: a mediation analysis of inflammatory biomarkers. Front Immunol. 2022;13:1080782. doi:10.3389/fimmu.2022.1080782
36. Ruffilli A, Neri S, Manzetti M, et al. Epigenetic factors related to low back pain: a systematic review of the current literature. Int J Mol Sci. 2023;24(3):1854. doi:10.3390/ijms24031854
37. Lis AM, Black KM, Korn H, et al. Association between sitting and occupational LBP. Eur Spine J. 2007;16(2):283–298. doi:10.1007/s00586-006-0143-7
38. Senthil P, Sudhakar S, Porcelvan S, et al. Implication of posture analysing software to evaluate the postural changes after corrective exercise strategy on subjects with upper body dysfunction-a randomized controlled trial. J Clin Diagn Res. 2017;11(7):Yc01–yc04. doi:10.7860/JCDR/2017/26520.10229
39. Phimphasak C, Swangnetr M, Puntumetakul R, et al. Effects of seated lumbar extension postures on spinal height and lumbar range of motion during prolonged sitting. Ergonomics. 2016;59(1):112–120. doi:10.1080/00140139.2015.1052570
40. Steffens D, Maher CG, Pereira LS, et al. Prevention of low back pain: a systematic review and meta-analysis. JAMA Intern Med. 2016;176(2):199–208. doi:10.1001/jamainternmed.2015.7431
41. Dhawan S, Andrews R, Kumar L, et al. A randomized controlled trial to assess the effectiveness of muscle strengthening and balancing exercises on chemotherapy-induced peripheral neuropathic pain and quality of life among cancer patients. Cancer Nurs. 2020;43(4):269–280. doi:10.1097/NCC.0000000000000693
42. Fischer SC, Calley DQ, Hollman JH. Effect of an exercise program that includes deadlifts on low back pain. J Sport Rehabil. 2021;30(4):672–675. doi:10.1123/jsr.2020-0324
43. Vanti C, Andreatta S, Borghi S, et al. The effectiveness of walking versus exercise on pain and function in chronic low back pain: a systematic review and meta-analysis of randomized trials. Disabil Rehabil. 2019;41(6):622–632. doi:10.1080/09638288.2017.1410730
44. Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389(10070):736–747. doi:10.1016/S0140-6736(16)30970-9
45. Shiri R, Coggon D, Falah-Hassani K. Exercise for the prevention of low back pain: systematic review and meta-analysis of controlled trials. Am J Epidemiol. 2018;187(5):1093–1101. doi:10.1093/aje/kwx337
46. Budhrani-Shani P, Berry DL, Arcari P, et al. Mind-body exercises for nurses with chronic low back pain: an evidence-based review. Nurs Res Pract. 2016;2016:9018036. doi:10.1155/2016/9018036
47. Jordan JL, Holden MA, Mason EE, et al. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. 2010;2010(1):Cd005956. doi:10.1002/14651858.CD005956.pub2
48. Hackney AC. Stress and the neuroendocrine system: the role of exercise as a stressor and modifier of stress. Expert Rev Endocrinol Metab. 2006;1(6):783–792. doi:10.1586/17446651.1.6.783
49. Wegner M, Helmich I, Machado S, et al. Effects of exercise on anxiety and depression disorders: review of meta- analyses and neurobiological mechanisms. CNS Neurol Disord Drug Targets. 2014;13(6):1002–1014. doi:10.2174/1871527313666140612102841
50. Hall AM, Kamper SJ, Maher CG, et al. Symptoms of depression and stress mediate the effect of pain on disability. Pain. 2011;152(5):1044–1051. doi:10.1016/j.pain.2011.01.014
51. Azfar SM, Murad MA, Azim SR, et al. Frequency of and various factors associated with stress, anxiety, and depression among low back pain patients. Cureus. 2019;11(9):e5701. doi:10.7759/cureus.5701
52. Ikeda T, Cooray U, Suzuki Y, et al. Changes in body mass index on the risk of back pain: estimating the impacts of weight gain and loss. J Gerontol a Biol Sci Med Sci. 2022;78(6):973–979. doi:10.1093/gerona/glac184
53. Nitecki M, Shapiro G, Orr O, et al. Association between BMI and non-specific recurrent low back pain in over 600,000 healthy young adults. Am J Epidemiol. 2023;192(8):1371–1378. doi:10.1093/aje/kwad102
54. Gallagher KM, Callaghan JP. Early static standing is associated with prolonged standing induced low back pain. Hum Mov Sci. 2015;44:111–121. doi:10.1016/j.humov.2015.08.019
55. Özcan-Ekşi EE, Kara M, Berikol G, et al. A new radiological index for the assessment of higher body fat status and lumbar spine degeneration. Skeletal Radiol. 2022;51 (6) :1261–1271 doi:10.1007/s00256-021-03957-8.
56. Berikol G, Ekşi MŞ, Aydın L, et al. Subcutaneous fat index: a reliable tool for lumbar spine studies. Eur Radiol. 2022;32(9):6504–6513. doi:10.1007/s00330-022-08775-7
57. Orenius T, Silén E, Nuortimo A, et al. Psychological interventions in preventing chronicity of sub-acute back pain: a systematic review. Scand J Pain. 2022;22(2):211–217. doi:10.1515/sjpain-2021-0063
58. Kim JY, Shin JS, Lim MS, et al. Relationship between simultaneous exposure to ergonomic risk factors and work-related lower back pain: a cross-sectional study based on the fourth Korean working conditions survey. Ann Occup Environ Med. 2018;30:58. doi:10.1186/s40557-018-0269-1
59. Pinheiro MB, Morosoli JJ, Ferreira ML, et al. Genetic and environmental contributions to sleep quality and low back pain: a population-based twin study. Psychosom Med. 2018;80(3):263–270. doi:10.1097/PSY.0000000000000548

