Cancer and neoplasms
Role of colectomy in the management of appendiceal tumors: a retrospective cohort study
Practice patterns by type of operation
In total, there were 18,216 appendiceal tumors in the study group, including 1,970 (11%) GCA, 6,219 (34%) mucinous adenocarcinoma, 5,603 (31%) NEN, and 4,424 (24%) non-mucinous adenocarcinoma tumors. A majority of all patients were treated with RHC (60%). Overall, RHC was most frequently performed in GCA (69%) and least frequently performed in NEN (46%) (Table 1).
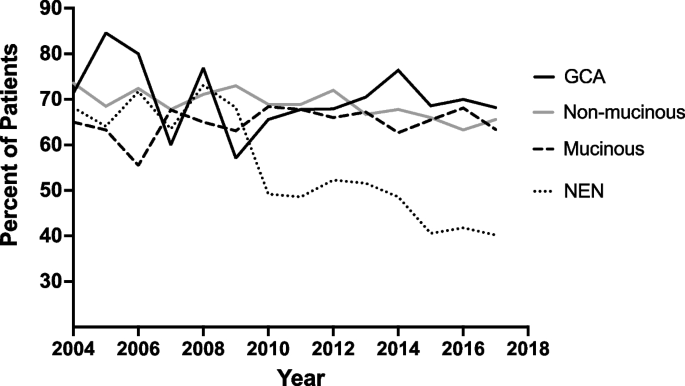
The trend in rate of RHC over time varied considerably by tumor type (Fig. 2). Rate of RHC was approximately constant over the study period for mucinous and non-mucinous adenocarcinoma at around 60–70%. RHC for GCA was initially labile, ranging from a peak of 85% of surgeries for GCA in 2005 to a nadir of 57% in 2009, before reaching a plateau of about 70% from 2015–2017. RHC for NEN decreased dramatically over the study period, from 68% of cases in 2004 to 40% of cases in 2017 (p = 0.008).
Annual proportion of patients with appendiceal cancer receiving right hemicolectomy stratified by histologic type. Abbreviations: GCA, Goblet cell adenocarcinoma; NEN, Neuroendocrine neoplasm
Predictors of right hemicolectomy
Predictors of RHC varied by type of tumor (Table 2). Stage of disease and facility location were significant predictors of extent of surgery for all tumor types.
For GCA, cases treated in the West were 40% less likely to undergo RHC than cases treated in the Northeast (OR: 0.6, 95% CI: 0.4–0.9, p = 0.005). Stage 2 (OR: 1.5, 95% CI: 1.2–2.0, p < 0.001), stage 3 (OR: 3.4, 95% CI: 2.2–5.4, p < 0.001), and stage 4 (OR: 1.7, 95% CI: 1.1–2.6, p = 0.013) disease were significantly more likely to be treated with RHC than stage 1 tumors.
For mucinous adenocarcinoma, cases treated in the Midwest were 30% more likely to receive RHC than those treated in the Northeast (OR: 1.3, 95% CI: 1.1–1.5, p = 0.006). Stage 3 cases were 60% more likely to be treated with RHC (OR: 1.6, 95% CI: 1.2–2.1, p < 0.001) compared to stage 1 cases. Moderately differentiated (OR: 1.3, 95% CI: 1.2–1.5, p < 0.001) and poorly-differentiated (OR: 1.4, 95% CI: 1.2–1.7, p < 0.001) tumors were more likely to undergo RHC than well-differentiated tumors. Tumors with lymphovascular invasion were also significantly more likely to undergo RHC (OR: 1.3, 95% CI: 1.1–1.5, p = 0.012), as were cases diagnosed in 2011 or after rather than before.
For NEN, patients with age ≥ 65 were more likely to undergo RHC (OR: 1.3, 95% CI: 1.1–1.6, p = 0.006), as were those with a Charlson-Deyo score of 1 (OR: 1.3, 95% CI: 1.1–1.5, p = 0.008) or ≥ 2 (1.4, 95% CI: 1.1–1.9, p = 0.012) rather than 0. Cases treated in the West were 30% less likely to undergo RHC than cases treated in the Northeast (OR: 0.7, 95% CI: 0.6–0.9, p = 0.004). Stage 2 (OR: 4.2, 95% CI: 3.6–5.0, p < 0.001), stage 3 (OR: 6.8, 95% CI: 5.6–8.4, p < 0.001), and stage 4 (OR: 3.1, 95% CI: 2.4–4.0, p < 0.001) tumors were significantly more likely to be treated with RHC than stage 1 tumors. Moderately differentiated (OR: 1.3, 95% CI: 1.0–1.7, p = 0.032) tumors and tumors with lymphovascular invasion (OR: 1.5, 95% CI: 1.3–1.8, p < 0.001) were significantly more likely to be treated with RHC.
For non-mucinous adenocarcinoma, patients diagnosed 2011–2017 were 20% less likely to undergo RHC than those diagnosed 2004–2010 (OR: 0.8, 95% CI: 0.7–1.0, p = 0.015). Cases treated in the West were 30% less likely to undergo RHC than cases treated in the Northeast (OR: 0.7, 95% CI: 0.6–0.9, p = 0.003). Stage 3 tumors (OR: 1.6, 95% CI: 1.3–2.1, p < 0.001) were significantly more likely to be treated with RHC than stage 1 tumors. Moderately differentiated tumors were also significantly more likely to undergo RHC (OR: 1.2, 95% CI: 1.0–1.5, p = 0.022).
Patient outcomes and survival analysis by type of operation
Surgical outcomes of appendectomy and RHC stratified by tumor type and stage are presented in Table 3. Negative surgical margins were more common after RHC than after appendectomy for all stages and all tumor types, although the difference did not reach statistical significance for some smaller subgroups. The disparity in overall negative surgical margin rate was greatest for stage 2 disease, in which appendectomy yielded negative margins in 83% of cases (all cancer types) compared to 93% for RHC cases (p < 0.001). For stage 3 GCA, appendectomy resulted in negative margins in only 61% of cases, compared to 86% of RHC cases (p = 0.003).
RHC was also associated with longer inpatient stays compared to appendectomy for the group as a whole (median 5 days vs. 3 days, p < 0.001). A higher proportion of RHC cases resulted in unplanned readmission for all tumor types except non-mucinous adenocarcinoma and for the study group as a whole. For patients with NEN, RHC was associated with higher 30-day mortality (1.2% vs. 0.6%, p = 0.049) and 90-day mortality (3% vs. 1%, p = 0.004).
On risk-adjusted survival analysis, patients who underwent RHC experienced statistically significant longer overall survival than patients who underwent appendectomy for stage 2 disease no matter the histologic type, with the strongest benefit observed in GCA (HR: 0.43, 95% CI: 0.28–0.65, p < 0.001) and the least benefit observed in NEN (HR: 0.61, 0.39–0.95, p = 0.030). A mortality benefit with RHC was also seen in stage 1 and stage 4 non-mucinous adenocarcinoma (Fig. 3). Of note, patients with stage 1 NEN who underwent RHC had a significantly higher mortality than those that underwent appendectomy only (HR: 1.49, 1.11–1.99, p = 0.007).

Risk-adjusted hazard ratios associated with right hemicolectomy rather than appendectomy for each stage of each histologic type of appendiceal cancer. Abbreviations: RHC, Right hemicolectomy; CI, Confidence interval; S, Stage; appy, appendectomy