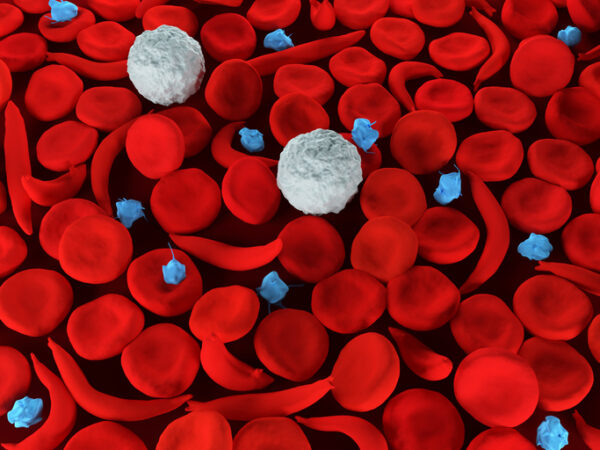
Blood
U.K. Is First to Approve a CRISPR-Based Therapy, Covering Two Blood Disorders
A novel gene-editing medicine is now authorized in the United Kingdom for treating two inherited blood disorders, a landmark decision that marks the first approval anywhere in the world for a therapy based on the CRISPR technology.
The Medicines and Healthcare products Regulatory Agency (MHRA) decision covers the treatment of patients 12 and older who have sickle cell disease or transfusion-dependent beta thalassemia. The therapy, known in development as exagamglogene autotemcel, or exa-cel, will be commercialized by Vertex Pharmaceuticals and CRISPR Therapeutics under the brand name Casgevy.
Both sickle cell disease and beta thalassemia stem from errors in the genes that code for hemoglobin, the oxygen-carrying proteins found on red blood cells. In sickle cell disease, the abnormal hemoglobin causes red blood cells to take on a crescent shape that causes ongoing complications such as severe pain, life threatening infections, and anemia. The few drugs available for sickle cell disease are chronic therapies.
The low levels of hemoglobin in beta thalassemia can lead to severe anemia. Patients require frequent blood transfusions, which introduces other complication risks. Stem cell transplants offer a potentially curative treatment option for both sickle cell disease and beta thalassemia. But the procedure requires a matched donor and it comes with the risk of rejection.
Casgevy is made by collecting a patient’s stem cells from the bone marrow. In a lab, CRISPR is used to edit a gene in those cells to produce high levels of fetal hemoglobin. Before these modified stem cells are administered, a conditioning regimen is required to kill the remaining cells in a patient that are making faulty hemoglobin. Infused into the patient, the modified stem cells make their way to the bone marrow. Patients may need to remain hospitalized for at least a month while those cells take up residence in the bone marrow and start producing red blood cells that incorporate fetal hemoglobin. Casgevy is intended to be a one-time treatment.
The MHRA decision is based on results from a trial in sickle cell disease that enrolled 45 patients. Of those, only 29 have been in the study long enough for the primary efficacy interim analysis. All but one of those patients were free of severe pain crises for at least 12 months after treatment.
In the beta thalassemia trial, 42 of 54 patients have been in the clinical trial long enough to be eligible for the primary efficacy interim analysis. Of those eligible patients, 39 did not need a red blood cell transfusion for at least 12 months after treatment with Casgevy. The remaining three patients showed a more than 70% reduction in the need for transfusions.
Side effects reported in the trials included nausea, fatigue, fever, and a high risk of infections. Those problems are similar to those for other autologous stem cell transplant procedures. No serious adverse effects were reported from the studies. The MHRA decision is a conditional marketing authorization valid for one year. Vertex and CRISPR Therapeutics are required to conduct additional post-marketing clinical research. The authorization for Casgevy may be renewed annually as long as ongoing review of real-world data and post-marketing studies continue to support use of the therapy.
“Today is a historic day in science and medicine: this authorization of Casgevy in Great Britain is the first regulatory authorization of a CRISPR-based therapy in the world,” Vertex CEO Reshma Kewalramani said in a prepared statement.
According to Vertex and CRISPR Therapeutics, the U.K. has an estimated 2,000 patients eligible for treatment with Casgevy. The MHRA said more details about the product’s label will be published on its website within a week.
U.K. approval of Casgevy comes ahead of upcoming regulatory decisions in the U.S. Last month, an FDA advisory committee gave its backing to the CRISPR-editing therapy. Casgevy faces a Dec. 8 target date for an FDA decision in sickle cell disease. In beta thalassemia, the therapy should receive an FDA decision by March 30, 2024.
In a note sent to investors, William Blair analyst Tim Lugo said Casgevy’s approval is an important milestone for people who have both blood disorders. He added that the regulatory decision is key validation for CRISPR Therapeutics’ deep pipeline of therapies based on CRISPR gene-editing. Using a model that assumes a price of $1.6 million for beta thalassemia and $1.5 million for sickle cell disease in Europe, William Blair projects peak sales of Casgevy in both indications topping $1.6 billion in Europe in the early 2030s.
A one-time treatment for beta thalassemia is already available from Bluebird Bio. Last year, Bluebird won FDA approval for Zynteglo, marking the first gene therapy approval in the rare blood disorder. That therapy carries a $2.8 million wholesale price. A different Bluebird gene therapy developed for sickle cell disease is expected to receive an FDA decision by Dec. 20.
Image: Meletios Verras, Getty Images