Congenital disorders
Paediatric postprocedural complications
Introduction
Surgery is one of the most important therapies provided by the National Health Service (NHS) in secondary care in the United Kingdom (UK).1 In the UK, a substantial proportion of NHS expenditure, activity, and mortality rates are attributed to the considerable volume of hospital procedures performed annually.2 In England alone, in 2022, the total number of procedures performed has reached 11,582,866 episodes.3 Globally, the annual volume of major surgical procedures conducted in 2012 was approximately 312.9 million, reflecting a substantial rise of 38.2% compared to the numbers recorded in 2004.4 Research indicates that postoperative complications can affect a range of patients, with estimates ranging from 7% to 44% among those undergoing major surgery.5–7 These complications have significant implications for both patients and the healthcare system.
Postoperative complications are a significant reason for patient mortality following surgical procedures.8,9 The overall rate reported for postoperative mortality varies between 0.79% and 5.7%.10 Research has revealed that the likelihood of a postoperative complication affects survival following major surgery more significantly than intraoperative events and preoperative risk factors.11 Moreover, postoperative complications result in extended hospital stays, elevated treatment expenses, diminished life expectancy, raised level of care required upon discharge, and reduced quality of life for patients who survive after hospitalization.10 These highlights evidence that comprehension of postoperative complications is essential for improving patient outcomes and optimizing the utilization of healthcare resources allocated to surgical care.
In general, compared to adult surgery, pediatric surgery is more challenging and has a higher incidence of complications. Age at surgery has an inverse relationship with intraoperative and postoperative problems.12 Age and surgical method can both affect the frequency of problems. A strong inflammatory response and poor compliance also increase the risk of postoperative complications. Due to the challenges in doing thorough postoperative tests on children, who may be recalcitrant, postoperative problems might be difficult to detect.12 Shock due to a severe drop in blood pressure, hemorrhage, wound infection, deep vein thrombosis, reaction to anesthesia, pulmonary embolism, and lung difficulties due to a lack of deep breathing and coughing exercises within 48 hours of surgery are also common postoperative consequences. Inhaling food, water, or blood into the airways can also cause these symptoms.13
Even with advanced surgical techniques and the expertise of skilled surgeons, effectively managing post-surgical complications has consistently posed the most prominent challenge in patient care.14 Pediatric patients undergoing surgical procedures or medical interventions represent a vulnerable population with unique healthcare needs. Postprocedural complications in this cohort can significantly impact their outcomes and quality of life. Understanding the patterns of postprocedural complications hospitalization for pediatric patients is essential for improving patient care and safety. No prior studies have investigated postprocedural complications in pediatric patients in England and Wales. Therefore, this study aims to analyze the hospitalization patterns associated with postprocedural complications among the pediatric population in England and Wales over the past two decades.
Materials and Methods
Study Sources and the Population
This was an ecological study using hospital admission data for all National Health Service (NHS) trusts and any independent sector funded by NHS trusts. Data were extracted from the Hospital Episode Statistics (HES) database in England15 and the Patient Episode Database for Wales (PEDW) for the period between April 1999 and April 2020.16 These two medical databases were used previously to examine hospitalisation pattern of different clinical outcomes and diseases.17–23 Postprocedural complications related hospital admissions were identified using the 10th version of the International Statistical Classification of Diseases (ICD) system (D78, E89, H59, H95, J95, L76, M96, and N99.24 The HES and PEDW databases record all hospital admissions, outpatient encounters and Accident and Emergency activities performed at all NHS trusts and any independent sector funded by NHS trusts. For research purposes, the HES database is a valid and trusted resource. On a regular basis, the data entry and quality tests are assessed and enhanced. The data utilized by the HES are extracted from discharge summaries and clinical notes. Each trust is tasked with the responsibility of having trained clinical coders input the data in accordance with a national data standard. An annual audit is conducted on a restricted subset of cases, during which clinical audits are compared with data from the HES. The information is systematically collected and encoded at every single facility. Following this, the documents are transferred to Digital Health Care in Wales via electronic means, where they are verified and incorporated into the main database. To calculate the annual hospital admission rate, we collected mid-year paediatric population data for the period between 1999 and 2020 from the Office for National Statistics (ONS).25 Then, for each ICD code, the number of hospitalisation episodes for each year was divided by the pediatric population in the same year.
Ethical Approval
Hospital admissions and population data are publicly available as anonymised data. Therefore, there was no need to obtain ethical approval for the study.
Statistical Analysis
Quantitative counts of hospitalization episodes are accessible in both databases. For each ICD code, stratified by age, hospitalization episodes are reported. Hospital admissions rates were calculated with their 95% confidence intervals (CIs) using the absolute number of admissions for paediatric patients divided by the mid-year paediatric population of the same year. The confidence interval was estimated using the following equation for the population proportion: p^ + / − z*(p^(1 − p^)/n).0.5 The Chi-squared test to assess the difference between the hospital admission rates. A two-sided p<0.05 was considered statistically significant. All analyses were performed using SPSS software version 27 (IBM Corp, Armonk, NY, USA).
Results
Overall Hospitalization Profile
The annual number of hospital admissions for postprocedural complications and disorders across various systems witnessed a 6.2% increase, rising from 824 in 1999 to 875 in 2020. During the same period, the rate of hospital admissions declined by 2.1% [from 8.32 (95% CI 7.75–8.88) per 100,000 persons in 1999 to 8.15 (95% CI 7.61–8.68) per 100,000 persons in 2020, p>0.05].
The primary reasons for hospital admissions associated with postprocedural complications were related to the respiratory system (Tracheostomy complications, acute pulmonary insufficiency following thoracic surgery, acute pulmonary insufficiency following nonthoracic surgery, chronic pulmonary insufficiency following surgery, chemical pneumonitis due to anesthesia, postprocedural subglottic stenosis, intraoperative hemorrhage and hematoma of a respiratory system organ or structure complicating a procedure, and accidental puncture and laceration of a respiratory system organ or structure during a procedure), genitourinary system (Postprocedural (acute) (chronic) kidney failure, postprocedural urethral stricture, postprocedural adhesions of vagina, prolapse of vaginal vault after hysterectomy, postprocedural pelvic peritoneal adhesions, complications of stoma of urinary tract, intraoperative hemorrhage and hematoma of a genitourinary system organ or structure complicating a procedure, and accidental puncture and laceration of a genitourinary system organ or structure during a procedure), and ear and mastoid process (Recurrent cholesteatoma of postmastoidectomy cavity, other disorders of ear and mastoid process following mastoidectomy, intraoperative hemorrhage and hematoma of ear and mastoid process complicating a procedure, accidental puncture and laceration of ear and mastoid process during a procedure, postprocedural hemorrhage of ear and mastoid process following a procedure, and postprocedural hematoma and seroma of ear and mastoid process following a procedure), constituting 43.0%, 23.8%, and 23.0% of cases, respectively (Table 1).
|
Table 1 Percentage of Hospital Admission from the Total Number of Admission |
The Change in Hospital Admissions Rates for Postprocedural Complications
Over the course of the past two decades, there has been a notable increase in hospital admissions rates for postprocedural complications and disorders related to the respiratory system, genitourinary system, and musculoskeletal system. Specifically, the rates for postprocedural complication have risen by 52.2. The rates for postprocedural complications related to respiratory system disorders, genitourinary system disorders, and musculoskeletal system disorders have climbed by 24.5% and 17.9%, respectively. However, it is worth noting that the hospital admissions rate for postprocedural complications related to disorders of eye and adnexa, the ear and mastoid process, as well as endocrine and metabolic complications and disorders, shown a significant drop of 63.5%, 49.8%, and 36.6%, correspondingly, as illustrated in Table 2 and Figure 1.
|
Figure 1 Trends of hospital admission stratified by type. |
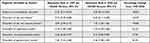 |
Table 2 Percentage Change in the Hospital Admission Rates |
Discussion
The findings of this ecological study highlight the trends in hospital admissions for postprocedural disorders among pediatric patients in England and Wales over two decades. These findings underscore the importance of understanding the factors driving changes in pediatric healthcare utilization and post-surgical complications.
One of the primary findings of this study is that the annual number of hospital admissions for postprocedural disorders across various systems witnessed a 6.2% increase, rising from 824 in 1999 to 875 in 2020. Several factors could contribute to this increase in hospital admissions for postprocedural complications in pediatric patients in England and Wales.
Firstly, the increase in the overall pediatric population. From 1999/2000 to 2019/2020, the pediatric population below 15 years in England and Wales increased by 8.4%, rising from 9,908,100 to 10,742,440.26 As this population grows, it naturally results in increased healthcare utilization, with more individuals requiring medical care, surgeries, or procedures, ultimately increasing the number of admissions for postprocedural disorders.
Secondly, surgery outcomes are expected to be more sever for rural and socioeconomically disadvantaged populations.27 Therefore, the growing proportion of children living in poverty and facing deprivation in the UK28 may contribute to increased hospital admissions due to postprocedural disorders among pediatric patients. These children often face barriers to timely and preventive healthcare, leading to the development of more severe health conditions, including those necessitating surgical procedures. Consequently, this could lead to an elevated incidence of post-surgical complications.
Thirdly, advances in medical technology might have led to performing more complex procedures for pediatric patients, potentially increasing the likelihood of complications.29 Additionally, the epidemiologic shift from communicable to chronic and non-communicable conditions28 may also contribute to the rise in admissions. Noncommunicable disorders usually require more complex and long-term management, including procedures. This epidemiologic shift in the disease can increase the likelihood of hospitalization. Moreover, the growing prevalence of risk factors like poor dietary habits and sedentary lifestyles among children in the UK28 can lead to health issues that require medical intervention. These risk factors may contribute to conditions that result in increased postprocedural complications.
It is important to note that previous studies have identified several factors that are associated with postoperative outcomes, including geographic area,30 hospital location (urban versus rural),31 and insurance status.32–34
Contrary to the increase in the number of admissions, our study found that during the same period, the rate of hospital admissions for postprocedural disorders in pediatric patients declined by 2.1% [from 8.32 (95% CI 7.75–8.88) per 100,000 persons in 1999 to 8.15 (95% CI 7.61–8.68) per 100,000 persons in 2020, p>0.05]. Although the admissions rate has not decreased significantly, it has not increased parallel with the absolute number of admissions. However, we must continue to monitor these trends, as even a stable rate can indicate a significant condition burden, especially when considering the potential severity of complications in pediatric patients.
Our study revealed that the primary reasons for hospital admissions associated with postprocedural disorders among pediatric patients were related to the respiratory system (43.0%), genitourinary system (23.8%), and ear and mastoid process (23.0%) (Table 1). These findings underscore the importance of healthcare professionals focusing on these specific systems when developing preventative and management strategies for postprocedural disorders. Individualized treatments, improved monitoring, and enhanced patient education may be advantageous to reduce the incidence and severity of postprocedural issues within these systems.
Postoperative respiratory complications likewise emerge as a significant concern across various age groups and regions. The most common postoperative complications in Thailand were respiratory insufficiency and pneumonia.35 Moreover, a previous study found that respiratory failure was the most common complication in patients undergoing intra-abdominal operations.36 Besides, several trends across research suggest that pulmonary complications tend to surpass cardiac complications in frequency,36–38 emphasizing the significance of postoperative respiratory failure as the most prevalent type of postoperative pulmonary complication.39,40
Over the course of the past two decades, there has been a notable increase in hospital admissions rates for postprocedural disorders related to the respiratory system, genitourinary system, and musculoskeletal system. Specifically, the rates for postprocedural respiratory system disorders have risen by 52.2%. In addition, the rates for the postprocedural of genitourinary system disorders, and musculoskeletal system disorders have climbed by 24.5% and 17.9%, respectively. These trends underscore the growing importance of addressing and managing postprocedural complications in these systems within the healthcare system.
As previously discussed, several factors may contribute to the rise in admissions for postprocedural complications, encompassing factors such as the growth of the pediatric population, childhood poverty rates, disparities in healthcare access, epidemiological shifts, and other factors. All these factors can result in increased frequency and/or complexity of procedures related to the respiratory system, genitourinary system, or musculoskeletal system performed, accordingly increasing related postprocedural complications. It is crucial to address child poverty, enhance healthcare access and quality, promote preventive care, and manage pertinent risk factors to improve child health outcomes in England and Wales.
Between 1999 and 2020 in England, the total number of finished consultant episodes involving procedures and interventions related to the respiratory tract among patients aged below 15 years increased by 2.17-fold from 22,259 to 70,614.41,42 Furthermore, from 1999 to 2019, hospital admission rates for respiratory system diseases and “musculoskeletal and connective tissue diseases” among patients aged below 15 years in England and Wales saw substantial increases of 34.0%43 and 45.9%,44 respectively. Additionally, in line with our findings, intra-operative and post-procedural complications and disorders of the musculoskeletal system-related hospital admission rates among patients aged below 15 years increased by 17.9% in England and Wales.45
Hospital admission rates for postprocedural disorders related to the eye and adnexa, ear and mastoid process, as well as endocrine and metabolic systems, have shown significant reductions of 63.5%, 49.8%, and 36.6%, respectively. These findings could suggest advancements in medical care, prevention, preoperative and postoperative care, or procedural techniques in these regions over the study period.
A prior study conducted from 1999 to 2019 found a 1.4% increase in hospital admissions related to eye and adnexal diseases among patients under 15 years old in England and Wales.46 The contrasting trends of decreased postprocedural disorder admissions for eye and adnexal diseases and increased admissions for eye and adnexal diseases among patients under 15 years old in England and Wales suggest an improvement in the safety and effectiveness of surgical interventions and medical procedures targeting the eye and adnexal over the study duration.
Furthermore, according to a previous statistical, from 1999 to 2020 in England, there was a significant decline in the total number of finished consultant episodes involving procedures and interventions related to the ear, eye, and endocrine systems among patients aged below 15 years. The numbers decreased by 51.6% (from 52,844 to 25,554), 20.9% (from 19,850 to 15,698), and 3.8% (from 552 to 531), respectively.41,42 These statistics align with our results, further emphasizing the improvements in healthcare delivery and favorable patient outcomes in procedures related to the ear, eye, and endocrine systems over the study period.
Recommendations
Enhanced Preventative Measures
Healthcare providers should consider enforcing targeted preventative criteria to manage pediatric postprocedural complications, specifically in healthcare systems that have seen significant increases in admission rates, including respiratory, musculoskeletal, and genitourinary systems. These criteria could include enhancing preprocedural assessments and implementing stringent intra- and post-procedural monitoring protocols.
Research and Evidence-Based Interventions
It is essential to continuously investigate the specific causes and risk factors behind these trends to facilitate the development of evidence-based treatments. As such, collaborative efforts among healthcare institutions, researchers, and policymakers are needed to establish standardized guidelines and recommendations for pediatric therapies, thus ensuring the highest patient safety level.
Education and Awareness Programs
Develop programs for parents, caregivers, and medical professionals to increase awareness of post-operative difficulties as well as the significance of early intervention.
Continuing Professional Development
Encourage healthcare providers to participate in continuous professional development to stay updated on advancements in pediatric surgery and medical treatment.
This study his limitations. The utilization of aggregated data at the population level posed challenges in conducting patient follow-ups and identifying important confounding variables. This may have resulted in an underestimation or overestimation of our hospitalization rate. The utilization of aggregated data has imposed limitations on the ability to obtain crucial patient demographic information, such as comorbidities and ethnicity. The available data refers to the entire population and consists of aggregated information on hospitalizations, categorized by age and presented as absolute numbers. The freely available pediatric population data in the databases lack gender-stratified statistics. Gender stratification is available for the whole population only. This limited our ability to present hospitalisation rate for each specific ICD sub-code stratified by gender and age. Unfortunately, the absence of patient-level data has impeded our capacity to compute age-standardized hospitalization rates. It is crucial to recognize that the absence of individual-level data hinders the ability to accurately determine the magnitude of variation. Hence, it is imperative to exercise caution when interpreting our findings.
Conclusion
The incidence of postprocedural complications among the pediatric population has been consistent throughout the course of the last two decades. In the pediatric population, postprocedural complications primarily led to hospital admissions for conditions involving the respiratory system, genitourinary system, ear, and mastoid process. The significance of continuously monitoring the hospitalization trend for this particular issue stems from the progress made in healthcare delivery and the need to enhance patient care and safety. Further research is warranted to investigate gender-related disparities pertaining to postprocedural complications and ascertain significant modifiable risk factors.
Data Sharing Statement
Publicly available datasets were analyzed in this study. This data can be found here: http://http//content.digital.nhs.uk/hes, http://www.infoandstats.wales.nhs.uk/page.cfm?pid=41010&orgid=869
Ethics Approval and Informed Consent
The study was approved by the Institutional Review Board at Isra University, Amman, Jordan gave their clearance with IRB No. SREC/22/08/84. This study was conducted in accordance with the World Medical Association (WMA) Declaration of Helsinki
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
This work was supported and funded by the Deanship of Scientific Research at Imam Mohammad Ibn Saud Islamic University (IMSIU) (grant number IMSIU-RP23022).
Author Contributions
Conceptualization, A.Y.N. and H.A.; methodology, A.Y.N.; validation, A.Y.N., formal analysis, A.Y.N.; investigation, A.Y.N. and H.A.; data curation, A.Y.N. and H.A.; writing—original draft preparation, A.Y.N. and H.A.; writing—review and editing, A.Y.N. and H.A.; supervision, A.Y.N. and H.A.; project administration, A.Y.N. and H.A.; funding acquisition, H.A. All authors have read and agreed to the published version of the manuscript. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported and funded by the Deanship of Scientific Research at Imam Mohammad Ibn Saud Islamic University (IMSIU) (grant number IMSIU-RP23022).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Royal College of Surgeons England. Surgery and the NHS in numbers; 2023. Available from: https://www.rcseng.ac.uk/news-and-events/media-centre/media-background-briefings-and-statistics/surgery-and-The-nhs-in-numbers/. Accessed January 28, 2023.
2. Abbott TEF, Fowler AJ, Dobbs TD, Harrison EM, Gillies MA, Pearse RM. Frequency of surgical treatment and related hospital procedures in the UK: a national ecological study using hospital episode statistics. Br J Anaesth. 2017;119(2):249–257. doi:10.1093/bja/aex137
3. National Health Services. Hospital Admitted Patient Care Activity 2021–22; 2023. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity/2021-22. Accessed January 28, 2023.
4. Weiser TG, Haynes AB, Molina G, et al. Size and distribution of the global volume of surgery in 2012. Bull World Health Organ. 2016;94(3):201. doi:10.2471/BLT.15.159293
5. Jakobson T, Karjagin J, Vipp L, et al. Postoperative complications and mortality after major gastrointestinal surgery. Medicina. 2014;50(2):111–117. doi:10.1016/j.medici.2014.06.002
6. Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Eng j Med. 2009;360(5):491–499. doi:10.1056/NEJMsa0810119
7. Tevis SE, Cobian AG, Truong HP, Craven MW, Kennedy GD. Implications of multiple complications on the postoperative recovery of general surgery patients. Ann Surg. 2016;263(6):1213. doi:10.1097/SLA.0000000000001390
8. Klohnen A. New perspectives in postoperative complications after abdominal surgery. Vet Clin North Am Equine Pract. 2009;25(2):341–350.
9. Pearse RM, Harrison DA, James P, et al. Identification and characterisation of the high-risk surgical population in the United Kingdom. Critical Care. 2006;10(3):1–6.
10. Tevis SE, Kennedy GD. Postoperative complications and implications on patient-centered outcomes. j surgi res. 2013;181(1):106–113. doi:10.1016/j.jss.2013.01.032
11. Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, Kumbhani DJ. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242(3):326. doi:10.1097/01.sla.0000179621.33268.83
12. Trivedi RH, Wilson ME. Intraoperative and Postoperative Complications. In: Khokhar SK, Dhull C, editors. Essentials of Pediatric Cataract Surgery. Singapore: Springer Singapore; 2022:61–74.
13. Johns Hopkins Medicine. After surgery: discomforts and complications; 2023. Available from: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/after-surgery-discomforts-and-complications. Accessed January 28, 2023.
14. Ali MZ. Assessment of postoperative complications in abdominal surgeries by Clavein-Dindo Classification System in the Indian hospital setting. Acad J Surg. 2021;4:16–21.
15. Health and Social Care Information Centre (HSCIC). Hospital Episode Statistics; 2021. Available from: http://http//content.digital.nhs.uk/hes. Accessed March 01, 2021.
16. NHS Wales Informatics Service. Annual PEDW Data Tables; 2021. Available from: http://www.infoandstats.wales.nhs.uk/page.cfm?pid=41010&orgid=869. Accessed March 01, 2021.
17. Hemmo SI, Naser AY, Alwafi H, et al. Hospital admissions due to ischemic heart diseases and prescriptions of cardiovascular diseases medications in England and Wales in the past two decades. Int J Environ Res Public Health. 2021;18(13):7041. doi:10.3390/ijerph18137041
18. Naser AY, Wang Q, Wong LYL, et al. Hospital admissions due to dysglycaemia and prescriptions of antidiabetic medications in England and Wales: an ecological study. Diabetes Ther. 2018;9(1):153–163. doi:10.1007/s13300-017-0349-1
19. Mustafa Ali MK, Naser AY, AbuAlhommos A, et al. Hospital admissions secondary to diseases of the blood, blood-forming organs, and immune system in England and Wales. Cureus. 2022;14(10):e30179. doi:10.7759/cureus.30179
20. Mustafa Ali S, Naser AY, Alghanemi AG, et al. Musculoskeletal system and connective tissue related hospital admission in England and Wales between 1999 and 2019: an ecologic study. Cureus. 2022;14(12):e32453. doi:10.7759/cureus.32453
21. Naser AY, Al-shehri H. Admissions due to perinatal respiratory and cardiovascular disorders in England. J Multidiscip Healthc. 2023;16:199–207. doi:10.2147/JMDH.S396406
22. Naser AY, Al-Shehri H, Altamimi N, Alrasheed A, Albalawi L. Profile of hospital admissions due to preterm labor and delivery in England. Healthcare. 2023;11(2).
23. Naser AY, Dahmash EZ, Alqahtani JS, Alsairafi ZK, Alsaleh FM, Alwafi H. Trends in hospital admissions for mental, behavioural and neurodevelopmental disorders in England and Wales between 1999 and 2019: an ecological study. Healthcare. 2022;10(11):2191.
24. ICD10Data.com. 2021 ICD-10-CM Codes; 2021. Available from: https://www.icd10data.com/ICD10CM/Codes. Accessed March 01, 2021.
25. Office for National Statistics (ONS). Population estimates; 2021 Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland. Accessed March 01, 2021.
26. ONS. UK population estimates, 1838; 2020. Available from: https://www.ons.gov.uk/file?uri=/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland/mid2001tomid2020detailedtimeseries/ukpopulationestimates18382020.xlsx., Accessed November 14,2023.
27. Torain MJ, Maragh-Bass AC, Dankwa-Mullen I, et al. Surgical disparities: a comprehensive review and new conceptual framework. J Am Coll Surg. 2016;223(2):408–418. doi:10.1016/j.jamcollsurg.2016.04.047
28. Wolfe I, Sigfrid L, Chanchlani N, Lenton S. Child health systems in the United Kingdom (England). J Pediatr. 2016;177:S217–S242. doi:10.1016/j.jpeds.2016.04.058
29. England NHS, Improvement NHS. Paediatric critical care and surgery in children review: summary report 2019; 2022.
30. Harounian JA, Schaefer E, Schubart J, Carr MM. Pediatric adenotonsillectomy and postoperative hemorrhage: demographic and geographic variation in the US. Int J Pediatr Otorhinolaryngol. 2016;87:50–54. doi:10.1016/j.ijporl.2016.05.018
31. McAteer JP, Richards MK, Stergachis A, et al. Influence of hospital and patient location on early postoperative outcomes after appendectomy and pyloromyotomy. J Pediatr Surg. 2015;50(9):1549–1555. doi:10.1016/j.jpedsurg.2015.03.063
32. Duval M, Wilkes J, Korgenski K, Srivastava R, Meier J. Causes, costs, and risk factors for unplanned return visits after adenotonsillectomy in children. Int J Pediatr Otorhinolaryngol. 2015;79(10):1640–1646. doi:10.1016/j.ijporl.2015.07.002
33. Mowrer AR, Esparaz JR, Nierstedt RT, et al. Failure to thrive: the socioeconomics of pediatric gastrostomy complications. J Pediatr Surg. 2020;55(5):855–860. doi:10.1016/j.jpedsurg.2020.01.017
34. Stone ML, LaPar DJ, Mulloy DP, et al. Primary payer status is significantly associated with postoperative mortality, morbidity, and hospital resource utilization in pediatric surgical patients within the United States. J Pediatr Surg. 2013;48(1):81–87. doi:10.1016/j.jpedsurg.2012.10.021
35. Sakornpant P, Kojaranjit V. First National Congenital Cardiac Surgical Database Report: demonstrating “Practice of Congenital Cardiac Surgery in Thailand: analysis of Performance and Outcome”; 2014.
36. Thompson JS, Baxter BT, Allison JG, Johnson FE, Lee KK, Park WY. Temporal patterns of postoperative complications. Arch Surg. 2003;138(6):596–603. doi:10.1001/archsurg.138.6.596
37. Lawrence VA, Hilsenbeck SG, Noveck H, Poses RM, Carson JL. Medical complications and outcomes after Hip fracture repair. Arch Intern Med. 2002;162(18):2053–2057. doi:10.1001/archinte.162.18.2053
38. Khan NA, Quan H, Bugar JM, Lemaire JB, Brant R, Ghali WA. Association of postoperative complications with hospital costs and length of stay in a tertiary care center. J Gen Intern Med. 2006;21(2):177–180. doi:10.1007/s11606-006-0254-1
39. Canet J, Sabate S, Mazo V, et al. Development and validation of a score to predict postoperative respiratory failure in a multicentre European cohort: a prospective, observational study. Eur J Anaesthesiol. 2015;32(7):458–470. doi:10.1097/EJA.0000000000000223
40. Mazo V, Sabate S, Canet J, et al. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiol. 2014;121(2):219–231. doi:10.1097/ALN.0000000000000334
41. NHS. Hospital admitted patient care activity, 2019–20: procedures and interventions; 2020. Available from: https://files.digital.nhs.uk/20/0864E6/hosp-epis-stat-admi-proc-2019-20-tab.xlsx. Accessed November 14, 2023.
42. NHS. Hospital episode statistics, admitted patient care – England, 1999-00: main operations summaries; 2000. Available from: https://files.digital.nhs.uk/publicationimport/pub03xxx/pub03973/hosp-epis-stat-admi-main-ops-sum-99-00-tab.xls. Accessed November 14, 2023.
43. Naser AY, Mansour MM, Alanazi AFR, et al. Hospital admission trends due to respiratory diseases in England and Wales between 1999 and 2019: an ecologic study. BMC Pulm Med. 2021;21(1):1–10. doi:10.1186/s12890-021-01736-8
44. Ali SM, Naser AY, Alghanemi AG, et al. Musculoskeletal system and connective tissue related hospital admission in England and Wales between 1999 and 2019: an Ecologic Study. Cureus. 2022;14(12). doi:10.7759/cureus.32453
45. Hashem M. Intraoperative and post-procedural complications and disorders of musculoskeletal system hospitalization profile in England and Wales. CEGH. 2023;20:101252. doi:10.1016/j.cegh.2023.101252
46. Alrawashdeh HM, Naser AY, Alwafi H, et al. Trends in hospital admission due to diseases of the eye and adnexa in the past two decades in England and Wales: an ecological study. Int J Gen Med. 2022:1097–1110. doi:10.2147/IJGM.S344380

