Cardiovascular
Screening onset of acute coronary syndromes
Department of Cardiology, Intervention Cardiology Center, Wuhan No.1 Hospital, Wuhan, 430022, People’s Republic of China
Correspondence: Liqun He, Department of Cardiology, Intervention Cardiology Center, Wuhan No.1 Hospital, No. 215, Zhongshan Avenue, Qiaokou District, Wuhan, 430022, People’s Republic of China, Tel/Fax +86-027-85332105, Email [email protected]
Purpose: Acute coronary syndrome (ACS) is a common acute myocardial ischemia syndrome and is one of the death-related causes of cardiovascular diseases. Identifying biomarkers to indicate disease severity and predict the occurrence of major adverse cardiovascular events (MACE) would benefit the clinical prognosis of ACS. This study estimated the expression and significance of lncRNA TPRG1-AS1 in the onset and development of ACS, aiming to explore a novel biomarker for the diagnosis and prognosis of ACS.
Patients and Methods: A total of 109 ACS patients and 66 patients who received coronary angiography and excluded ACS were enrolled in this study. TPRG1-AS1 in the serum of study subjects was analyzed by PCR. The significance of TPRG1-AS1 in screening ACS was evaluated by ROC analysis. The association of TPRG1-AS1 with the disease severity of ACS was assessed by Pearson correlation analysis with patients’ clinicopathological features. The potential of TPRG1-AS1 in predicting the occurrence of MACE was assessed by logistic regression analysis.
Results: Significant upregulation of TPRG1-AS1 was observed in ACS patients, which served as a risk factor for ACS and distinguish between ACS patients and the normal group. TPRG1-AS1 was positively correlated with Gensini score, cys-C, cTnI, and NT-proBNP levels of ACS patients, which indicate severe development of ACS. Additionally, increasing serum TPRG1-AS1 was associated with the high incidence of MACE during patients’ hospitalization and was identified as a risk factor for MACE in ACS patients.
Conclusion: Upregulated TPRG1-AS1 in ACS served as a diagnostic biomarker and predicted the severe development of patients.
Introduction
Acute coronary syndrome (ACS) is a common cardiovascular disease with high incidence, many complications, and high mortality. Atherosclerosis is the pathological basis of ACS, where the plaque is invaded or ruptured leading to the formation of a thrombus in the lumen and causing the stenosis or occlusion of the coronary lumen.1 With the aging of the population, ACS has become a major disease that followed malignant tumors and dramatically threatens human health. The diagnosis of ACS is mainly based on clinical symptoms, electrocardiogram findings, and levels of myocardial necrosis markers.2 The severity of coronary artery disease needs to be evaluated by coronary angiography. There are various complications of ACS, such as arrhythmia, hypotensive shock, cardiogenic shock, heart failure, and other cardiac dysfunction induced by cardiac cell death, which promote disease development and increase severity. Severe complications would induce lung infections. However, the diagnosis of ACS and the evaluation of complications depend on contrast medium, which is unfriendly for allergy, hyperthyroidism, renal dysfunction, and other special patients, and the costs are relatively high.3,4 Therefore, there is an urgent need to explore novel biomarkers to screen ACS and indicate disease severity.
Non-coding RNAs (ncRNAs) have been widely reported to participate in the onset and development of cardiovascular diseases. ncRNAs would show differential expression under different pathological conditions. Long non-coding RNAs (lncRNAs) are critical members of ncRNAs with a length of over 200 nt. Previous studies have reported the role of lncRNA in cardiovascular diseases and identified a series of candidate lncRNA biomarkers for ACS.5 A previous transcriptome study identified a number of dysregulated lncRNAs in coronary artery diseases (CAD), among which lncRNA TPRG1-AS1 (ENST00000444488.1) was found to discriminate CAD patients and diagnose the occurrence of acute myocardial infarction.6 TPRG1-AS1 is the antisense RNA of TPRG1 located on chromosome 3. Additionally, TPRG1-AS1 was recently revealed to regulate vascular smooth muscle cells and further regulate atherogenesis.7 TPRG1-AS1 was also identified as a prognostic biomarker of head and neck squamous cell carcinoma and promoted the development of human cancers.8–10 Therefore, TPRG1-AS1 was speculated to be involved in the pathogen and development of ACS, which lacks confirmed data in current reports. Serum TPRG1-AS1 level can be analyzed by PCR assay, which could provide a rapid quantification. Compared with the controversial vascular examination, the cost of PCR is low, and the analysis cycle is quick. Hence, serum TPRG1-AS1 level could provide a convenient biomarker for ACS.
In this study, the expression and significance of TPRG1-AS1 in the early detection and outcome prediction of ACS were assessed, aiming to identify a novel biomarker for the diagnosis and severity evaluation of ACS.
Materials and Methods
Patients
This study had been approved by the Ethics committee of Wuhan No.1 Hospital (No. 2020114) and was performed in line with the principles of the Declaration of Helsinki. A total of 109 ACS patients enrolled in this study according to the following criteria: 1) patients meet the diagnostic criteria of ACS according to the diagnosis guideline;11 2) patients were confirmed by the coronary angiography; 3) the clinical records are completed; 4) patients were informed of the study design and signed informed consent. Another 66 patients who received coronary angiography and excluded ACS were enrolled as the normal group. Patients with one of the following items were excluded: 1) patients who had received coronary artery bypass grafting or thrombolysis; 2) ACS patients induced by the coronary myocardial bridge, coronary spasm, coronary artery fistula, tachyarrhythmia, and bradyarrhythmia; 3) patients with malignant tumors, metabolic diseases, autoimmune disease, and liver or kidney dysfunction; 4) pregnant women.
To avoid the effects of complications and basic diseases, the baseline information of the two groups, including age, gender, history of smoking and drinking, disease history, and blood lipid indicators.
Sample Collection
Fasting elbow venous blood was collected from all study subjects early in the morning. Blood samples were analyzed with the automatic biochemical analyzer to obtain blood indexes. The serum was isolated by centrifugation at 3500 rpm for 10 min and stored at −80°C until further analyses.
Follow-Up Survey
ACS patients were followed up during their hospitalization to summarize the occurrence of major adverse cardiovascular events (MACE), including all-reason deaths, revascularization, nonfatal myocardial infarction, and cardiac death.
Real-Time Quantitative PCR
Total RNA was extracted using Trizol reagent (Invitrogen, USA) and assessed by the ratio of OD260/280. cDNA was generated with isolated RNA using Transcript ALL-in-One First-Strand cDNA Synthesis SuperMix kit (Life Technologies, USA). PCR amplification was performed with SYBR Green kit (Applied Biosystem, USA) on the 7500 PCR system (Applied Biosystem, USA). The relative expression of TPRG1-AS1 was calculated by the 2−ΔΔCT method with β-Actin as the internal reference.
Statistical Analyses
The difference comparison between the two groups was performed with a Student’s t-test (P 0.5). The correlation of TPRG1-AS1 with ACS patients’ disease severity was estimated by its correlation with patients’ clinicopathological features by Pearson correlation analysis.
Results
Baseline Information of Study Subjects
ACS patients showed matched age and gender composition with the normal group. The normal group included 34 male patients and 32 female patients with an average age of 58.56 ± 9.51 years, while ACS patients were composed of 57 males and 52 females with an average of 58.42 ± 9.89 years. There were no significant differences in BMI, habits of smoking and drinking, history of hypertension and diabetes, TC, TG, LDL, and HDL between the normal group and ACS patients (P > 0.05, Table 1). ACS patients showed significantly increasing levels of Gensini score, cys-c, cTnI, and NT-proBNP compared with the normal group (P < 0.001, Table 1).
|
Table 1 Baseline Information of Study Subjects |
Expression and Significance of TPRG1-AS1 in the Onset of ACS
Significant upregulation of serum TPRG1-AS1 was observed in ACS patients relative to the normal group (Figure 1a). Meanwhile, TPRG1-AS1 (P = 0.002) and HDL (P = 0.024) were both identified as risk factors for ACS according to the logistic regression analysis (Figure 1b). Consistently, based on the serum level of TPRG1-AS1, the ROC curve confirmed its significance in discriminating ACS patients with the cutoff of 1.145 (AUC = 0.858, Figure 1c).
 |
Figure 1 Expression and significance of TPRG1-AS1 in ACS. (a). TPRG1-AS1 was upregulated in ACS relative to the normal group. (b and c). TPRG1-AS1 was identified as a risk factor for ACS (b) and could discriminate ACS patients from the normal group (c). ****P < 0.0001. |
Association of TPRG1-AS1 with ACS Severity and the Occurrence of MACE
Among the significantly changed indicators, TPRG1-AS1 showed significantly positive correlations with ACS patients’ Gensini score (r = 0.870, Figure 2a), cys-c (r = 0.830, Figure 2b), cTnI (r = 0.888, Figure 2c), and NT-proBNP (r = 0.838, Figure 2d), which indicate the severe development of ACS patients.
|
Figure 2 Correlation of serum TPRG1-AS1 levels with the disease severity of ACS patients. TPRG1-AS1 was positively correlated with ACS patients’ Gensini score (r = 0.870, a), cys-C (r = 0.830, b), cTnI (r = 0.888, c), and NT-proBNP (r = 0.838, d). |
Additionally, according to the average serum TPRG1-AS1 levels in ACS patients, there were a low-TPRG1-AS1 group and a high-TPRG1-AS1 group established. The high-TPRG1-AS1 group showed a high incidence of MACE during their hospitalization (log-rank P = 0.025, Figure 3). TPRG1-AS1 was also demonstrated to be a risk factor for the occurrence of inpatient MACE of ACS patients with the OR value of 10.343 (P = 0.033), suggesting the promoted effect of increasing TPRG1-AS1 on adverse outcomes of ACS patients (Table 2).
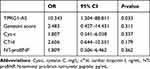 |
Table 2 Risk Factors for the Occurrence of MACE Evaluated by Logistic Regression Analysis |
|
Figure 3 Kaplan-Meier curve of ACS patients based on the serum level of TPRG1-AS1 (the occurrence of MACE was defined as the endpoint). Patients with relatively high TPRG1-AS1 expression showed a high occurrence of MACE than that of patients with relatively low TPRG1-AS1 expression. log rank P = 0.025. |
Discussion
ACS is an acute pathological type of coronary artery disease, of which the onset is acute, the condition is severe, and the prognosis is poor. It is essential for the early detection and prevention of ACS to constantly explore novel diagnostic and therapeutic techniques. In the clinic, there were a number of studies carried out for early warning of ACS, aiming to reduce the occurrence of cardiovascular events. Age, gender, smoking, history of hypertension, and many other clinicopathological features have been considered risk factors for ACS associated with disease onset.12–14 However, these indicators cannot help in judging and predicting the severity of the disease.15 Recently, the potential of biomarkers in disease screening and development prediction has been widely accepted. TPRG1-AS1 is a functional lncRNA in human diseases. For example, TPRG1-AS1 could sponge miR-4691-5p and miR-3659 and further regulate RBM24 and therefore suppress the progression of liver cancer.8 The transcription of TPRG1-AS1 was promoted by TFAP2A, which affected the glycolysis and angiogenesis of bladder urothelial carcinoma.9 The regulatory effect of TPRG1-AS1 was also observed in vascular smooth muscle cells, which attenuated atherogenesis.7 Herein, TPRG1-AS1 was upregulated in ACS, which was identified as a risk factor for ACS. Upregulated TPRG1-AS1 could distinguish between ACS patients and healthy individuals with relatively high sensitivity and specificity.
Meanwhile, the upregulation of TPRG1-AS1 was associated with increasing levels of Gensini score, cyc-c, cTnI, and NT-proBNP. Quantifying the severity of coronary disease is the basic premise of related research. Gensini score is employed to quantitatively evaluate the stenosis degree of coronary vascular in the clinic, which could indicate the disease severity of ACS patients.16–18 Cys-c is an endogenous cysteine protease inhibitor and participates in inflammation by interfering with the chemotaxis and phagocytosis of granulocytes. Under hypoxia and ischemia conditions, cys-C produced by cardiomyocytes was released into the blood, contributing to coronary plaque damage and the progression of atherosclerosis by inducing inflammation.19–22 cTnI existed in cardiomyocytes and would release into blood cycle when cardiomyocytes are injured. cTnI is more stable than other indicators. NT-proBNP is the split product of BNP stimulated by cardiomyocytes. Currently, serum cTnI and NT-proBNP are commonly used for assessing the extent and severity of myocardial ischemia in the clinic.23–25 Therefore, the positive correlation of TPRG1-AS1 with these factors suggested its potential in predicting the severe development of ACS.
The occurrence of MACE is the major adverse factor for ACS prognosis. Although there were several indicators reported to be associated with MACE, the predictive value of those factors is limited.26–28 An increasing number of studies have been devoted to exploring biomarkers for the prediction of MACE. For example, the latest study identified circulating miR-411-5p as a biomarker for the occurrence of MACE in atrial fibrillation, which was associated with the cardiovascular death of patients.29 Plasma miR-142 was found to predict MACE in coronary artery disease patients who received percutaneous coronary intervention.30 According to above findings, TPRG1-AS1 was suggested to indicate the severe development of ACS. Hence, TPRG1-AS1 was hypothesized to predict the occurrence of MACE. The follow-up during hospitalization showed that elevated serum TPRG1-AS1 was associated with the increasing occurrence of MACE and was identified as a risk factor for MACE.
However, there are still some works needed further investigation. ACS includes unstable angina pectoris, acute non-ST elevation myocardial infarction, and acute ST-elevation myocardial infarction. This study has not confirmed the dysregulation of TPRG1-AS1 in specific types of ACS and the significance of TPRG1-AS1 in disease development. Due to the limited study period and hospital scale, this study enrolled study subjects from a single center and lacked a long-term follow-up to evaluate the significance of TPRG1-AS1 in predicting long-term prognosis of ACS patients. Therefore, further research would specify the subtypes of ACS with larger sample size from multiple centers and conduct long-term follow-up survey. Moreover, the onset and development of cardiovascular diseases involved the progression of various cells, such as cardiomyocytes, cardiac fibroblasts, vascular endothelial cells, macrophages, and vascular smooth muscle cells. The regulatory effect of TPRG1-AS1 on these cells could provide insights into the mechanism underlying the function of TPRG1-AS1 in ACS.
Conclusion
In conclusion, upregulated TPRG1-AS1 in ACS served as a biomarker for the onset and severe disease development. Increasing serum TPRG1-AS1 could also predict the occurrence of MACE in ACS patients. These findings provide a potential serum indicator for the screening and monitoring of ACS.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ahmadi A, Argulian E, Leipsic J, Newby DE, Narula J. From subclinical atherosclerosis to plaque progression and acute coronary events: JACC state-of-the-art review. J Am Coll Cardiol. 2019;74(12):1608–1617. doi:10.1016/j.jacc.2019.08.012
2. Smith JN, Negrelli JM, Manek MB, Hawes EM, Viera AJ. Diagnosis and management of acute coronary syndrome: an evidence-based update. J Am Board Fam Med. 2015;28(2):283–293. doi:10.3122/jabfm.2015.02.140189
3. Boyd B, Zamora CA, Castillo M. Managing adverse reactions to contrast agents. Magn Reson Imaging Clin N Am. 2017;25(4):737–742. doi:10.1016/j.mric.2017.06.008
4. Marraccini P, Bianchi M, Fommei E, et al. Contrast medium nephrotoxicity after renal artery and coronary angioplasty. Acta radiologica. 2010;51(4):462–466. doi:10.3109/02841851003629045
5. Wang L, Jin Y. Noncoding RNAs as biomarkers for acute coronary syndrome. Biomed Res Int. 2020;2020:3298696. doi:10.1155/2020/3298696
6. Li L, Wang L, Li H, et al. Characterization of LncRNA expression profile and identification of novel LncRNA biomarkers to diagnose coronary artery disease. Atherosclerosis. 2018;275:359–367. doi:10.1016/j.atherosclerosis.2018.06.866
7. Ren X, Zhu H, Deng K, et al. Long noncoding RNA TPRG1-AS1 suppresses migration of vascular smooth muscle cells and attenuates atherogenesis via interacting with MYH9 protein. Arterioscler Thromb Vasc Biol. 2022;42(11):1378–1397. doi:10.1161/ATVBAHA.122.318158
8. Choi JH, Kwon SM, Moon SU, et al. TPRG1-AS1 induces RBM24 expression and inhibits liver cancer progression by sponging miR-4691-5p and miR-3659. Liver Int. 2021;41(11):2788–2800. doi:10.1111/liv.15026
9. He J, Dong C, Zhang H, Jiang Y, Liu T, Man X. The oncogenic role of TFAP2A in bladder urothelial carcinoma via a novel long noncoding RNA TPRG1-AS1/DNMT3A/CRTAC1 axis. Cell Signal. 2023;102:110527. doi:10.1016/j.cellsig.2022.110527
10. Li Z, Qiu X, He Q, Fu X, Ji F, Tian X. CCND1-associated ceRNA network reveal the critical pathway of TPRG1-AS1-hsa-miR-363-3p-MYO1B as a prognostic marker for head and neck squamous cell carcinoma. Sci Rep. 2023;13(1):11831. doi:10.1038/s41598-023-38847-7
11. Kimura K, Kimura T, Ishihara M, et al. JCS 2018 guideline on diagnosis and treatment of acute coronary syndrome. Circ J. 2019;83(5):1085–1196. doi:10.1253/circj.CJ-19-0133
12. Chhabra ST, Kaur T, Masson S, et al. Early onset ACS: an age based clinico-epidemiologic and angiographic comparison. Atherosclerosis. 2018;279:45–51. doi:10.1016/j.atherosclerosis.2018.10.017
13. Kringeland E, Tell GS, Midtbø H, Igland J, Haugsgjerd TR, Gerdts E. Stage 1 hypertension, sex, and acute coronary syndromes during midlife: the Hordaland Health Study. Eur J Prev Cardiol. 2022;29(1):147–154. doi:10.1093/eurjpc/zwab068
14. Manfrini O, Cenko E, Bugiardini R. Gender differences in residual risk factors for major adverse cardiovascular events following ACS and how to bridge the gap. Curr Atheroscler Rep. 2020;22(11):65. doi:10.1007/s11883-020-00882-4
15. Yamamoto K, Natsuaki M, Morimoto T, et al. Coronary artery disease without standard cardiovascular risk factors. Am J Cardiol. 2022;164:34–43. doi:10.1016/j.amjcard.2021.10.032
16. Chen J, Zhang Y, Liu J, et al. Role of lipoprotein(a) in predicting the severity of new on-set coronary artery disease in type 2 diabetics: a Gensini score evaluation. Diab Vasc Dis Res. 2015;12(4):258–264. doi:10.1177/1479164115579004
17. Rampidis GP, Benetos G, Benz DC, Giannopoulos AA, Buechel RR. A guide for Gensini score calculation. Atherosclerosis. 2019;287:181–183. doi:10.1016/j.atherosclerosis.2019.05.012
18. Tanaka T, Miki K, Akahori H, et al. Comparison of coronary atherosclerotic disease burden between ST-elevation myocardial infarction and non-ST-elevation myocardial infarction: non-culprit Gensini score and non-culprit SYNTAX score. Clin Cardiol. 2021;44(2):238–243. doi:10.1002/clc.23534
19. Doganer YC, Aydogan U, Aydogdu A, et al. Relationship of cystatin C with coronary artery disease and its severity. Coron Artery Dis. 2013;24(2):119–126. doi:10.1097/MCA.0b013e32835b6761
20. van der Laan SW, Fall T, Soumaré A, et al. Cystatin C and cardiovascular disease: a Mendelian randomization study. J Am Coll Cardiol. 2016;68(9):934–945. doi:10.1016/j.jacc.2016.05.092
21. Wallentin L, Eriksson N, Olszowka M, et al. Plasma proteins associated with cardiovascular death in patients with chronic coronary heart disease: a retrospective study. PLoS Med. 2021;18(1):e1003513. doi:10.1371/journal.pmed.1003513
22. Wang GN, Sun K, Hu DL, Wu HH, Wang XZ, Zhang JS. Serum cystatin C levels are associated with coronary artery disease and its severity. Clin Biochem. 2014;47(16–17):176–181. doi:10.1016/j.clinbiochem.2014.07.013
23. Almeida R, Mariano L, Gavina C, et al. The value of NT-proBNP in early risk stratification of acute coronary syndromes. Port J Cardiol. 2006;25(1):71–75.
24. Fan J, Ma J, Xia N, Sun L, Li B, Liu H. Clinical value of combined detection of CK-MB, MYO, cTnI and plasma NT-proBNP in diagnosis of acute myocardial infarction. Clin Lab. 2017;63(3):427–433. doi:10.7754/Clin.Lab.2016.160533
25. Hamaya R, Yonetsu T, Kanaji Y, et al. Interrelationship in the prognostic efficacy of regional coronary flow reserve, fractional flow reserve, high-sensitivity cardiac troponin-I and NT-proBNP in patients with stable coronary artery disease. Heart Vessels. 2019;34(3):410–418. doi:10.1007/s00380-018-1260-z
26. Mal K, Kumar R, Mansoor F, et al. Risk of major adverse cardiovascular events in patients with rheumatoid arthritis. Cureus. 2020;12(12):e12246. doi:10.7759/cureus.12246
27. Simonetto M, Murthy SB. Major adverse cardiovascular events after intracerebral hemorrhage-it’s all about location, location, location. JAMA Netw Open. 2023;6(4):e235783. doi:10.1001/jamanetworkopen.2023.5783
28. Yang K, Liu W. Triglyceride and glucose index and sex differences in relation to major adverse cardiovascular events in hypertensive patients without diabetes. Front Endocrinol (Lausanne). 2021;12:761397. doi:10.3389/fendo.2021.761397
29. Nopp S, van der Bent ML, Kraemmer D, et al. Circulatory miR-411-5p as a novel prognostic biomarker for major adverse cardiovascular events in patients with atrial fibrillation. Int J Mol Sci. 2023;24(4):3861. doi:10.3390/ijms24043861
30. Tang QJ, Lei HP, Wu H, et al. Plasma miR-142 predicts major adverse cardiovascular events as an intermediate biomarker of dual antiplatelet therapy. Acta Pharmacol Sin. 2019;40(2):208–215. doi:10.1038/s41401-018-0041-7

