Congenital disorders
Bangladesh life expectancy highest in South Asia
Bangladesh has made significant progress in the health sector in 30 years compared to other South Asian countries and the country now has the best health status in the region.
As a result, the country has the highest life expectancy at birth and health life expectancy than other countries in the south Asian region– Bhutan, India, Nepal, and Pakistan.
Over the past 30 years from 1990, life expectancy in Bangladesh has increased from 58.2 to 74.6 years and age-standardised death rates have reduced by half in the country. On the other hand, mortality rates have reduced by more than half in the period.
The information came from the findings of a new Global Burden of Disease (GBD) Study titled “The burden of diseases and risk factors in Bangladesh, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019.”
Carried out by a group of researchers with the support of the Bill & Melinda Gates Foundation, these findings of the GBD study have been revealed in a research article published in an international journal– The Lancet Global Health.
The Institute for Health Metrics and Evaluation (IHME) conducts the GBD studies and the IHME is the initiative of the University of Washington, USA.
The GBD study shows that Bangladesh has made significant achievements in reducing mortality rates and health loss by more than half from 1990 to 2019.
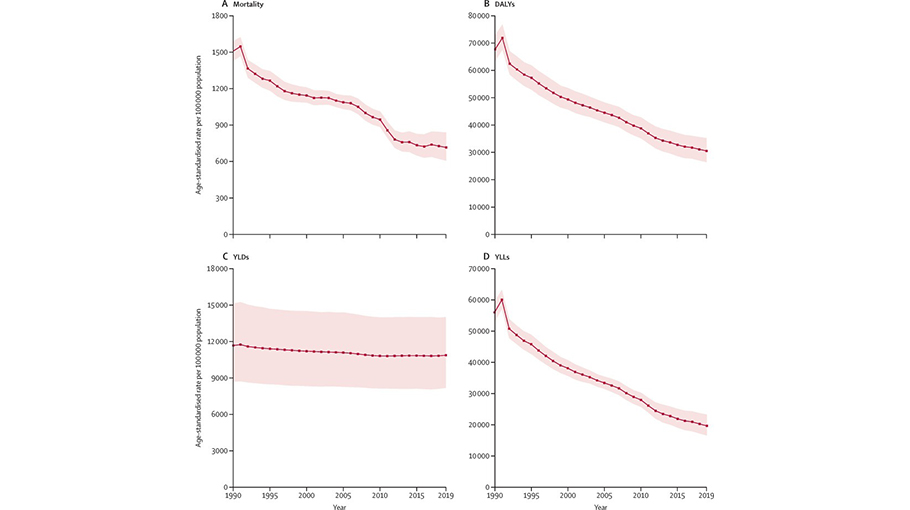
“Between 1990 and 2019, the age-standardised mortality rate decreased from 1509.3 to 714.4 deaths per 100000 populations. Bangladesh had the lowest rate of age-standardised mortality over the past 30 years within the south Asia region–Bhutan, India, Nepal, and Pakistan,” says the GBD study.
It also says that non-communicable diseases (NCDs), including hypertension, high glucose and smoking, were the major cause of death spurred by top risk factors. However, the prevalence of the NCDs, including stroke, ischaemic heart disease, COPD (chronic obstructive pulmonary disease), diabetes and chronic kidney disease; has increased steadily since 1990.
The researchers in their systematic review analysis show that the despite the increase of non-communicable diseases, the mortality rate has decreased significantly due to CMNN diseases (communicable, maternal, neonatal and nutritional diseases).
The researchers recommended that efforts are needed to implement cost-effective multi-sectoral programmes and strategies to prevent and control the NCDs and promote healthy lifestyles in both urban and rural areas.
The Global Burden of Disease (GBD) study provides a comprehensive picture of mortality and systematic analysis of disease burden and trends in Bangladesh. Some researchers and experts on public health in Bangladesh said that this study is the first on the issue.
Dr Shariful Islam, an associate professor and a physician scientist at the Institute for Physical Activity and Nutrition (IPAN) of Deakin University in Australia, and Adjunct Professor at Department of Noncommunicable Disease (NCD) at Bangladesh University of Health Sciences; led the research team and is the principal author of the article.
The other authors include Riaz Uddin, Subasish Das, Syed Imran Ahmed, Sojib Bin Zaman, Sheikh Mohammad Alif, Md Tanvir Hossen, Malabika Sarker, George Siopis, Sohel Reza Choudhury and Palash Chandra Banik.
Talking to the Daily Bangladesh Post on Friday (November 17), Dr Shariful Islam said that the increase in life expectancy is likely the results of improvements in maternal and child mortality as a result of improved health services and access to medicines funded by government, and high level of immunisation rates leading to prevention of communicable diseases.
“Bangladesh needs to prevent and control the increase in non-communicable diseases, which is caused in part by changing diets, sedentary behaviours, migration from rural to urban areas, changes in jobs from farming to office-based jobs and lack of healthcare support for prevention and rehabilitation of chronic diseases,” opined Dr Shariful Islam.
While commenting to the Daily Bangladesh Post about the findings of the study, Advocate Syed Mahbubul Alam Tahin, an expert on public health law and tobacco control; said that it is good news that the average life expectancy in Bangladesh has increased.
“It is a good achievement. Along with the achievement, it is desirable that people can enjoy this increase in life expectancy in good health. Emphasis should be placed to control non-communicable diseases (NCDs) as the NCDs is increasing in the country. For this reason, pollution free neat and clean environment and ecology must be ensured. Tobacco must be controlled,” said Advocate Syed Mahbubul Alam Tahin.
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 analysed the burden and trends of diseases and their risk factors in Bangladesh from 1990 to 2019, using the comprehensive GBD methodology.
Palash Chandra Banik, an Associate Professor at Department of NCD of Bangladesh University of Health Sciences (BUHS) in Dhaka who was involved in the study; told this correspondent that their study provides information to measure progress and achieve goals set by the Bangladesh government and other stakeholders.
Talking to the Daily Bangladesh Post, the expert on public health said that the findings of the research will play a vital role in achieving the target of the Sustainable Development Goals (SDGs) by 2030.
Dr. Dipak Kumar Mitra, a professor at the Department of Public Health in North South University; and Dr Malay Kanti Mridha, a professor at JPG School of Public Health of BRAC University; lauded the GBD study and the article published in The Lancet Global Health journal, saying that such kind of study is the first on the issue.
“The findings from the research article will be crucial and timely to guide the policy makers and programme managers of Bangladesh to establish health priorities, as the country is currently developing its fifth 5-year plan for the health, population, and nutrition sector,” said the two professors of public health.
The findings of the research reflect improved health-promotion activities and the increase in health-care service provision nationwide. However, Bangladesh still faces a double burden of communicable and non-communicable diseases. If the current trend continues, management of the increased burden of non-communicable diseases will be a considerable challenge for the country’s health system.
The research article says, “Bangladesh has made substantial progress in improving socioeconomic and health indicators over the past 50 years, but data on national disease burden are scarce.”
However, the country has made substantial health advances over the past 30 years despite spending less on health care than other countries in South Asia.
According to the GBD study, the total fertility rate among women of reproductive age in Bangladesh was 4.4 in 1990 and decreased consistently over the subsequent years to 1.8 in 2019.
In 1990, the life expectancy at birth was 58.2 years, which by 2019 had increased to 74.6 years.
Bangladesh also achieved a substantial improvement in HALE (health-adjusted life expectancy) between 1990 and 2019.
In 2019, non-communicable diseases represented 14 of the top 20 causes of death; the leading three causes were stroke, ischaemic heart disease, and chronic obstructive pulmonary disease.
High blood pressure, high fasting plasma glucose, and smoking were the top three risk factors. From 1990 to 2019, the rate of all-cause DALYs (disability-adjusted life years) decreased by 54.9%.
In 2019, the leading causes of DALYs and YLLs (years of life lost) were neonatal disorders, stroke, and ischaemic heart disease, whereas musculoskeletal disorders, depressive disorders, and low back pain were the leading causes of YLDs.
Bangladesh has the lowest age-standardised rates of mortality, YLDs, and YLLs and the highest life expectancy at birth in South Asia
The total number of people with non-communicable diseases increased from 95.5 million in 1990 to 145.0 million in 2019; while those with CMNN diseases (communicable, maternal, neonatal, and nutritional diseases) increased from 88.6 million to 104.9 million and those with injuries increased from 13.1 million to 28.9 million during the same period.
CMNN diseases contributed the most towards DALYs in Bangladesh. Neonatal disorders remained the top-ranked cause of DALYs between 1990 and 2019. DALYs from vaccine-preventable diseases decreased substantially between 1990 and 2019, as did DALYs due to other CMNN diseases such as diarrhoeal diseases, tuberculosis, typhoid, and paratyphoid.
DALYs attributed to nutritional disorders (such as protein-energy malnutrition) and injuries (including drowning and road injuries) decreased between 1990 and 2019.
The age-standardised all-cause mortality rate in Bangladesh was 714.4 deaths per 100000 populations in 2019.
Deaths due to non-communicable diseases increased between 1990 and 2019, with 14 of the top 20 leading causes of death in 2019 due to such diseases. Stroke was the leading cause of death throughout 1990–2019. However, the mortality rate due to stroke declined by 22.8% in this period.
Although the mortality rate due to diabetes increased between 1990 and 2010, this rate subsequently decreased during 2010–2019. Overall, deaths due to communicable diseases decreased substantially over the time.
Malaria was ranked as the tenth leading cause of death in 1990; however, by 2019, the associated mortality rate had decreased by 99.8% and malaria was ranked the 116th leading cause of death.
The mortality rate due to other vaccine-preventable diseases, including tetanus, diphtheria, and measles, also decreased between 1990 and 2019. However, deaths due to drowning decreased by 77.6% during this period.
In 1990, the rate of mortality in children younger than 5 years in Bangladesh was 132.9 deaths per 1000 livebirths. This rate decreased over subsequent years to 29.1 deaths per 1000 livebirths in 2019.
Neonatal disorders and lower respiratory infections were the top two causes of death in this age group in both 1990 and 2019. Other major causes of death in 2019 included congenital defects, typhoid and paratyphoid diseases, diarrhoeal diseases, and drowning.
Meanwhile, although the drowning rate has decreased since 1990, the country still has the highest rate of child drowning in South Asia.
The rate of age-standardised YLDs per 100000 population (representing the non-fatal burden) was 11,667.2 in 1990 and 10,865.3 in 2019–a decrease of 6.9% between these years.
In 2019, non-communicable diseases accounted for 13 of the 20 leading causes of YLDs. Musculoskeletal disorders, depressive disorders, low back pain, headache disorders, age-related hearing loss, dietary iron deficiency, blindness and vision loss, and gynaecological disorders all remained in the top ten leading causes of YLDs between 1990 and 2019.
During this period, the rates of YLDs attributed to neonatal disorders increased by 90.1%, tuberculosis decreased by 73.3% and road injuries decreased by 5.9%.
In 2019, of the top ten risk factors for all-cause mortality, five were metabolic, three were behavioural, and two were environmental and occupational. High systolic blood pressure was the leading metabolic risk factor for all-cause mortality.
Smoking, the leading behavioural risk factor, accounted for 12.1% of deaths. Household air pollution from solid fuels was the leading environmental and occupational risk factor and accounted for 11.1% of age-standardised all-cause mortality.
In 1990, of the top ten risk factors for all-cause DALYs, only one (high systolic blood pressure, ranked ninth) was a metabolic risk.
In 2019, high systolic blood pressure was also ranked as the number one risk factor, accounting for 10.7%.
Bangladesh ranked among the worst of the south Asian countries in terms of DALYs caused by stroke, diabetes, depressive disorders, and congenital defects. Most of the compared countries have a similar profile in terms of causes of age-standardised DALYs between 1990 and 2019, with neonatal disorders being among the top causes throughout these years.
However, Bangladesh ranks better than most other south Asian countries in terms of DALYs caused by tuberculosis, liver cirrhosis, and dietary iron deficiency disorder.
In 1990, the country ranked worst (fifth) within the compared countries in terms of life expectancy at birth; however, in 2019, the country had the highest life expectancy at birth and ranked first for HALE in South Asia.
In 1990, Bangladesh had the second-highest under-5 mortality rate of the compared countries in South Asia, with Nepal ranking first. However, over the years, this rate has decreased substantially in both countries.
In 2019, Bangladesh had the second-lowest under-5 mortality rate (after Nepal) in the region. In 2019, the country also had the lowest total fertility rate in South Asia. Health expenditure across the five countries differs considerably, with India and Pakistan spending the most and Bhutan spending the least.
Over the past three decades, the total number of deaths due to non-communicable diseases in Bangladesh has decreased. Despite this trend, non-communicable diseases remain a substantial cause of death and should be a health-care priority.
The prevalence and mortality rates of diabetes and breast cancer increased slightly, which is concerning and warrants further investigation.
Health loss attributed to the leading causes, as measured by DALYs, decreased between 1990 and 2019, with steep declines for protein-energy malnutrition, tetanus, measles, malaria, diarrhoeal diseases, and drowning.
This achievement might reflect successful public health policies and practices focused in those areas (eg, vaccination and sanitation programmes).
Diabetes and musculoskeletal disorders increased substantially from 1990 to 2019 and rose in ranking of the causes of health loss. Other areas of concern include stroke (ranked second in 2019), ischaemic heart disease (ranked third), and diabetes (ranked sixth).
Health loss due to tuberculosis, asthma, and COPD substantially reduced from 1990 to 2019, while smaller reductions were observed for road injuries and other malignant neoplasms.
Despite having tertiary facilities, services for non-communicable disease prevention and rehabilitation are insufficient in Bangladesh.
During the past three decades, the government of Bangladesh has worked to improve sanitation; provide safe drinking water, oral rehydration solution, and healthy diets and nutrients for children; promote high coverage of vaccines and use of insecticide-treated bednets; and improve maternal health services and pregnancy care.
This success can be attributed to Bangladesh’s pluralistic health-care system, involving participation from numerous national and international non-governmental organisations.
Bangladesh adopted a multisectoral action plan involving nearly 30 ministries and agencies to prevent and control non-communicable diseases from 2018 to 2025. Finally, road injuries and drowning remain considerable public health problems in Bangladesh and deserve more attention from policy makers.
In Bangladesh, life expectancy at birth has increased by more than 16 years since 1990, therefore increasing the ageing population.
The country is now experiencing an epidemiological transition from CMNN diseases towards non-communicable diseases and disabilities.
Multisectoral policies and practices prioritising the prevention and management of and rehabilitation from non-communicable diseases are mandatory to control the increase in mortality and morbidity.