Blood
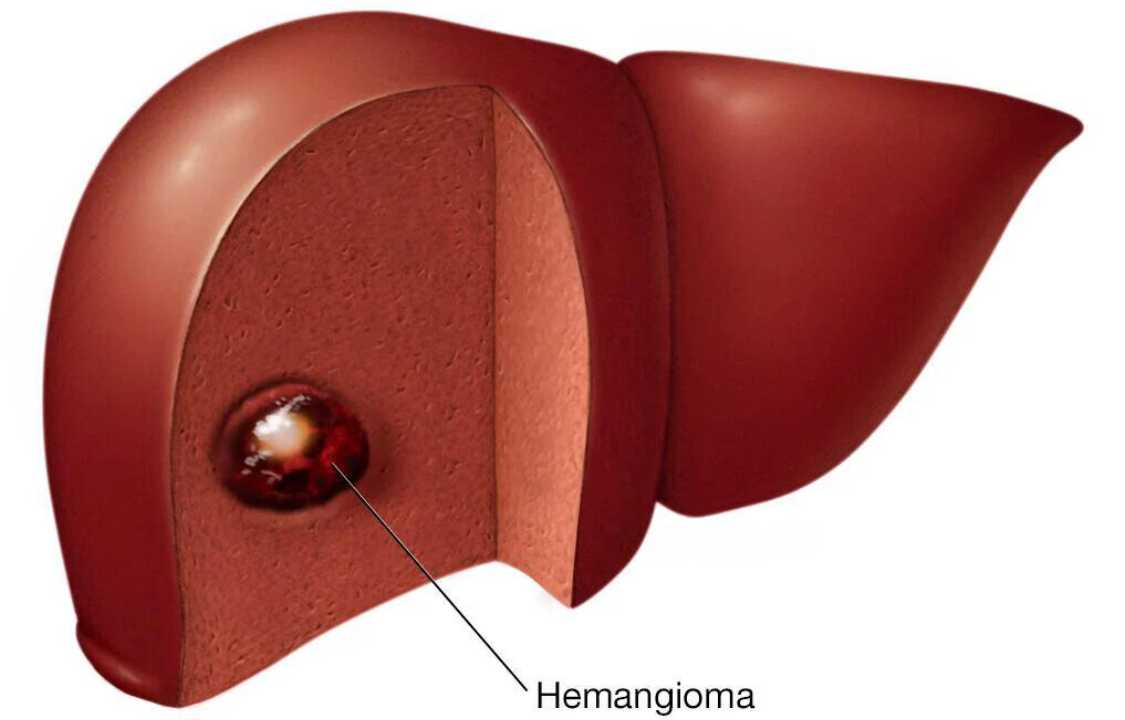
Liver Hemangioma
A liver hemangioma, also known as hepatic hemangioma or cavernous hemangioma, is a noncancerous (benign) mass within the liver characterized by a complex tangle of blood vessels. Despite its prevalence, affecting up to 20% of the population, liver hemangiomas are frequently discovered incidentally during imaging studies conducted for unrelated medical concerns. This article delves into the intricacies of liver hemangiomas, their characteristics, causes, risk factors, symptoms, diagnosis, potential complications, and treatment options, offering valuable insights to those affected by this condition.
Characteristics of Liver Hemangioma
A liver hemangioma presents itself as a mass composed of abnormal blood vessels that form a tangle within the liver tissue. These masses typically measure less than 1.5 inches (about 4 centimeters) in width, but larger or multiple hemangiomas can occur, although they are relatively rare. In many cases, liver hemangiomas remain dormant, causing no noticeable signs or symptoms, and they may remain this way throughout a person’s life. However, in some instances, liver hemangiomas can grow, potentially leading to symptoms that necessitate medical intervention.
Symptoms and When to Seek Medical Attention
Most individuals with liver hemangiomas do not experience any symptoms. However, when symptoms do manifest, they are generally non-specific and can be easily attributed to other causes. These symptoms may include:
1. Pain in the upper right abdomen
2. Early satiety (feeling full after eating only a small amount)
3. Nausea
4. Vomiting
If you experience persistent symptoms that concern you, it is advisable to consult a healthcare professional for an evaluation. While liver hemangiomas are often asymptomatic, it is crucial to rule out other potential underlying medical conditions.
Causes of Liver Hemangioma
The exact cause of liver hemangiomas remains unclear. It is widely believed that these abnormalities are congenital, meaning they are present from birth. Liver hemangiomas usually form as solitary collections of blood vessels within the liver, each measuring less than 1.5 inches in width. While they can occasionally be larger or occur in multiple clusters, this is relatively rare. The reason why some individuals develop symptomatic liver hemangiomas while others do not is not yet fully understood.
Risk Factors
Certain factors can increase the likelihood of being diagnosed with a liver hemangioma. These include:
1. Age: While liver hemangiomas can be diagnosed at any age, they are most commonly identified in individuals aged 30 to 50.
2. Gender: Women are more likely to be diagnosed with liver hemangiomas than men.
3. Pregnancy: Women who have been pregnant are at a higher risk of being diagnosed with a liver hemangioma. This increased risk is associated with elevated estrogen levels during pregnancy, which is believed to contribute to the growth of liver hemangiomas.
4. Hormone Replacement Therapy: Women using hormone replacement therapy for menopausal symptoms may also have an elevated risk of liver hemangioma diagnosis.
Potential Complications
Women diagnosed with liver hemangiomas may face complications during pregnancy due to the influence of estrogen, which tends to increase during this period and can cause some liver hemangiomas to grow larger. While becoming pregnant with a liver hemangioma is possible, it is essential to discuss potential complications with a healthcare provider to make informed decisions regarding pregnancy.
Additionally, medications that affect hormone levels, such as birth control pills, could potentially lead to an increase in the size of liver hemangiomas and pose complications. However, it’s important to note that this topic is subject to debate, and individuals considering such medications should consult their healthcare provider to assess the associated risks and benefits.
Diagnosis of Liver Hemangioma
Medical professionals utilize various diagnostic methods to identify liver hemangiomas, including:
1. Ultrasound: This imaging method employs high-frequency sound waves to create images of the liver.
2. Computerized Tomography (CT) Scanning: CT scans involve multiple X-ray images taken from different angles to produce cross-sectional images (slices) of the liver.
3. Magnetic Resonance Imaging (MRI): MRI utilizes a magnetic field and radio waves to generate detailed images of the liver.
4. Scintigraphy: A form of nuclear imaging that employs a radioactive tracer material to produce liver images.
The choice of diagnostic test depends on the specific clinical situation and the preferences of the medical team. In some cases, additional tests may be necessary for a comprehensive evaluation.
Treatment Options
If a liver hemangioma is small and remains asymptomatic, it typically does not require treatment. Most liver hemangiomas remain stable and do not grow. Nevertheless, healthcare providers may recommend periodic follow-up examinations to monitor the hemangioma for any potential growth, particularly if the mass is large.
Treatment decisions for liver hemangiomas are influenced by factors such as the size and location of the mass, whether multiple hemangiomas are present, the patient’s overall health, and individual preferences. Treatment options include:
1. Surgical Removal: If the liver hemangioma can be separated easily from the liver tissue, surgical removal may be recommended.
2. Partial Liver Resection: In cases where the hemangioma is closely integrated into the liver tissue, a partial liver resection may be necessary.
3. Procedures to Block Blood Flow: These interventions involve halting the blood supply to the hemangioma, causing it to shrink or stop growing. Two common methods include tying off the main artery (hepatic artery ligation) and injecting medication into the artery to block it (arterial embolization). These procedures preserve the surrounding healthy liver tissue.
4. Liver Transplant: In rare cases involving extensive or multiple hemangiomas that cannot be managed through other means, liver transplant surgery may be recommended. This entails removing the patient’s liver and replacing it with a donor liver.
5. Radiation Therapy: Radiation therapy employs high-energy beams, such as X-rays, to damage the cells of the hemangioma. However, it is rarely used due to the availability of safer and more effective treatment options.
Clinical trials and ongoing research may offer alternative treatments for liver hemangiomas, and individuals interested in participating in such trials should explore available options.
Preparing for Your Medical Appointment
Liver hemangiomas are often discovered incidentally during other medical tests or procedures. If you suspect you have a liver mass, you may be referred to a gastroenterologist or hepatologist. To prepare for your appointment and maximize its effectiveness, consider the following:
1. Be aware of any pre-appointment restrictions provided by the healthcare provider, such as dietary restrictions.
2. Document any symptoms you are experiencing, even if you suspect they are unrelated to your liver hemangioma, as this information can be valuable for your healthcare provider.
3. Compile a comprehensive list of all medications, vitamins, and supplements you are currently taking.
4. Bring a family member or friend along to the appointment to help you retain and recall the information discussed.
5. Develop a list of questions to ask your healthcare provider, which may include inquiries about the size of your liver hemangioma, whether you have multiple hemangiomas, potential growth of the hemangioma, necessary follow-up tests, treatment options, and any relevant printed materials or recommended websites.
6. Consider asking about medications that may worsen the condition, as well as inquiring about the relationship between your symptoms and the liver hemangioma.
Remember, your healthcare provider will also ask you questions during the appointment to gain a better understanding of your medical history and condition, so be prepared to discuss your symptoms, pregnancies, and any hormone replacement therapy use.
In Conclusion
A liver hemangioma is a benign mass of blood vessels within the liver that is often discovered incidentally. Although many individuals with liver hemangiomas remain asymptomatic and require no treatment, some may experience symptoms and require medical intervention. The cause of these masses remains unclear, but certain factors can increase the likelihood of diagnosis. Treatment options are available, ranging from surgical removal to blocking blood flow to the hemangioma or even liver transplant in rare cases.
Individuals diagnosed with liver hemangiomas should consult with their healthcare providers to determine the most appropriate course of action based on their specific circumstances. Ongoing research and clinical trials may yield new treatment options, offering hope for individuals affected by this condition,