Kidney
Vesicoureteral Reflux
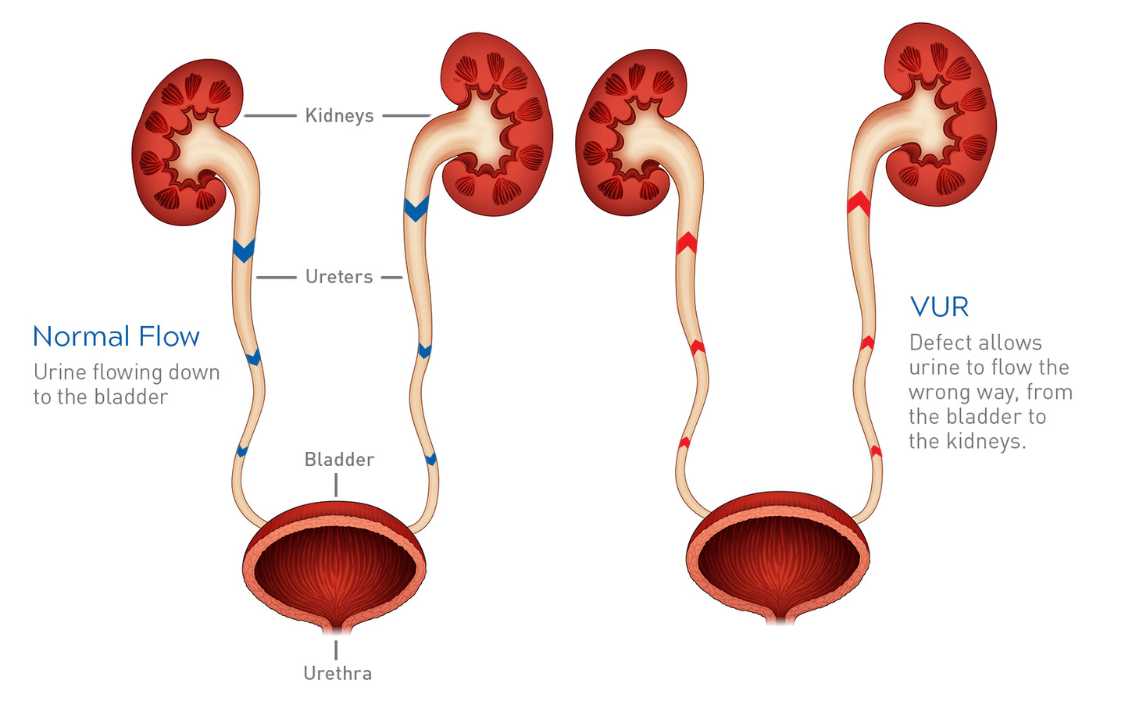
Vesicoureteral reflux (VUR) poses a complex challenge, particularly in the pediatric population, where early diagnosis and intervention are crucial. This condition disrupts the normal urinary flow, allowing urine to reflux from the bladder back into the ureters and potentially reaching the kidneys. The intricate interplay of the urinary system components, including the kidneys, ureters, bladder, and urethra, becomes compromised, leading to a cascade of symptoms and risks, especially in infants and children.
Vesicoureteral reflux (VUR) poses a considerable challenge to the normal physiological dynamics of the urinary system, where the seamless unidirectional flow of urine is disrupted. Ordinarily, urine follows a predetermined path, originating in the kidneys and traversing the ureters before reaching the bladder. However, in the intricate web of vesicoureteral reflux, this process takes an aberrant turn as urine regurgitates back into the ureters, prompting heightened concerns regarding its retrograde journey into the kidneys. This reversal of the urinary flow introduces a complexity that requires a nuanced and diligent approach to management, especially given that VUR can manifest across the lifespan but is predominantly diagnosed in the vulnerable demographic of infants and children. The delicate nature of pediatric cases underscores the necessity for an intricately tailored management strategy that considers the unique developmental aspects and potential long-term implications of vesicoureteral reflux in this specific population.
Clinical Presentation and Symptomatology
Timely identification of vesicoureteral reflux (VUR) is paramount for initiating prompt intervention and preventing potential complications. The primary clinical indicator often associated with VUR is urinary tract infections (UTIs), which can serve as a red flag for further investigation. However, diagnosing VUR through UTIs may be intricate, particularly in pediatric cases where the presentation might not adhere to conventional symptomatic patterns. The challenge lies in the fact that these infections may not always exhibit typical symptoms, adding a layer of complexity to the diagnostic process. In children and infants, subtle signs such as a persistent urge to urinate, a burning sensation during urination, cloudy urine, and abdominal or flank pain can be indicative of underlying vesicoureteral reflux. The nuances of pediatric symptoms, including unexplained fever, lack of appetite, and irritability, further underscore the importance of a comprehensive understanding of the diverse clinical presentations of VUR for accurate and timely diagnosis.
Long-Term Implications and Complications
The potential consequences of untreated vesicoureteral reflux extend beyond the immediate symptoms, with the risk of severe complications, notably kidney damage, looming large. The pathway to kidney damage is often paved by recurrent urinary tract infections (UTIs), which, when left unaddressed, can inflict permanent harm upon renal tissue, manifesting as kidney scarring. This scarring, if extensive, carries the ominous specter of complications such as hypertension, further escalating the medical ramifications. In the most severe instances, the relentless progression of kidney scarring may culminate in kidney failure, underscoring the critical need for proactive measures in managing vesicoureteral reflux. The correlation between the severity of reflux and the heightened likelihood of complications accentuates the significance of early detection and intervention, aiming not only to alleviate immediate symptoms but also to mitigate the long-term risks associated with untreated vesicoureteral reflux.
Diagnosis and Grading
Accurate diagnosis is essential for effective management. Urine tests, kidney and bladder ultrasound, and specialized X-rays of the urinary tract system contribute to a comprehensive diagnostic approach. Additionally, grading the severity of reflux, ranging from grade I to grade V, guides clinicians in tailoring appropriate interventions. Grade I represents the mildest form, where urine backs up only to the ureter, while grade V signifies severe kidney swelling and ureter twisting.
Individualized Treatment Approaches
The management of vesicoureteral reflux is nuanced and individualized, taking into account factors such as the age of the patient, the severity of reflux, and the presence of associated conditions. For mild cases, a watchful waiting approach may be appropriate, as some children may outgrow primary VUR. Medications, often antibiotics, play a crucial role in preventing UTIs and minimizing the risk of kidney damage.
In more severe cases, surgical intervention becomes a consideration. Open surgery, robotic-assisted laparoscopic surgery, and endoscopic surgery are among the options, each with its advantages and considerations. The choice of surgical approach is influenced by factors such as the age of the child, the extent of reflux, and the overall health of the patient.
Lifestyle Measures and Home Remedies
Beyond medical interventions, certain lifestyle measures can contribute to managing VUR. Encouraging adequate fluid intake, particularly water, helps dilute urine and flush out bacteria. Providing warmth through a heating pad or warm blanket can alleviate discomfort associated with UTIs.
For cases where bladder and bowel dysfunction (BBD) contribute to VUR, promoting healthy toileting habits becomes essential. Addressing constipation and ensuring regular emptying of the bladder can play a role in preventing UTIs and supporting overall urinary health.
The complexity of vesicoureteral reflux underscores the necessity for a holistic and individualized approach in addressing this urinary condition. Beyond the initial diagnosis and grading, the management of vesicoureteral reflux requires a multifaceted strategy that considers the unique characteristics of each case. This involves not only implementing established medical interventions such as medications or surgical procedures but also integrating innovative approaches that leverage advancements in medical science. The ongoing evolution of treatment strategies and surgical techniques reflects the commitment to enhancing patient outcomes and minimizing the impact of vesicoureteral reflux on individuals’ lives.
Moreover, recognizing the broader implications of vesicoureteral reflux, such as the risk of kidney damage and associated complications, emphasizes the importance of early detection and intervention. The potential for kidney scarring, hypertension, and kidney failure underscores the critical role that timely and targeted management plays in preventing severe consequences. Additionally, incorporating lifestyle measures, such as promoting adequate fluid intake and providing warmth to alleviate discomfort, contributes to a more comprehensive and patient-centric approach to vesicoureteral reflux management.
In summary, the dynamic landscape of vesicoureteral reflux management requires ongoing collaboration between healthcare providers, researchers, and patients. This collaborative effort aims not only to refine existing approaches but also to explore novel avenues that can further optimize outcomes and improve the overall quality of life for individuals affected by vesicoureteral reflux. By embracing a tailored and evolving strategy, healthcare professionals can continue to make significant strides in advancing the field of vesicoureteral reflux management and, ultimately, improving the well-being of those living with this condition.