Brain, Disorder, Mental Health
Epilepsy and the Corpus Callosotomy
Epilepsy, a neurological disorder characterized by recurrent seizures, can manifest in various forms, some of which are uncontrollable and life-altering. Among the myriad treatment options available, corpus callosotomy, sometimes referred to as split-brain surgery, stands as a profound intervention. This surgical procedure involves the severing of the corpus callosum, a bundle of nerve fibers deep within the brain that connects its two hemispheres. While it does not completely eliminate seizures, it curbs their severity and prevents them from spreading between the hemispheres. This article delves into the intricacies of corpus callosotomy, exploring its candidacy criteria, the procedure itself, its effectiveness, potential side effects, and risks.
Who Qualifies for a Corpus Callosotomy?
Corpus callosotomy is a surgical measure usually reserved for individuals with the most severe and uncontrollable forms of epilepsy, particularly when seizures affect both sides of the brain. Often, these are patients who have not responded to conventional treatments, such as antiseizure medications. This procedure is not the initial course of action but is considered when other therapeutic avenues have been exhausted.
Preparations for Corpus Callosotomy
Before a corpus callosotomy, candidates undergo a comprehensive evaluation. This pre-surgery assessment comprises multiple tests, including seizure monitoring, electroencephalography (EEG), magnetic resonance imaging (MRI), and positron emission tomography (PET). These diagnostic tools enable the medical team to pinpoint the origin of seizures and comprehend their propagation throughout the brain. They are also instrumental in determining whether a corpus callosotomy is a suitable intervention.
The Corpus Callosotomy Procedure
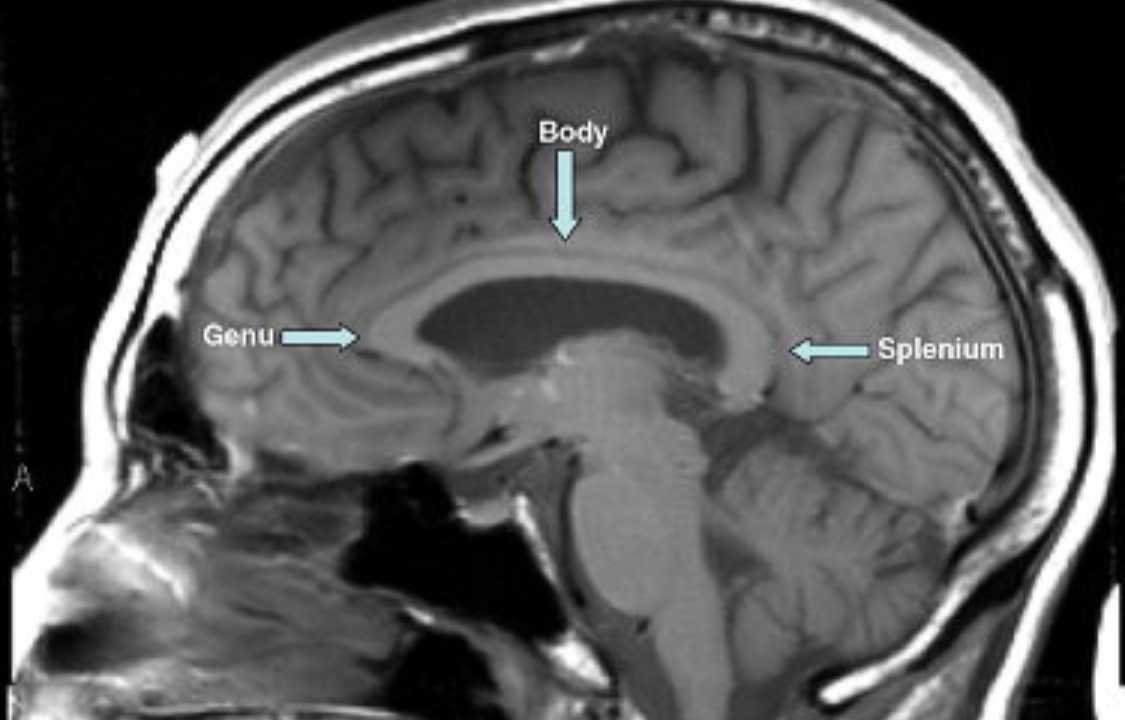
Corpus callosotomy necessitates a craniotomy, a surgical procedure to expose the brain. The patient is placed under anesthesia, ensuring they are unconscious during the operation. The surgeon initiates the procedure by making an incision in the scalp. Subsequently, a piece of bone is removed, and a portion of the dura, the protective membrane enveloping the brain, is gently retracted. This maneuver creates a surgical “window” through which specialized instruments are introduced to disconnect the corpus callosum. The surgeon then meticulously separates the hemispheres, with the aid of surgical microscopes providing an amplified view of the brain structures.
In certain cases, a corpus callosotomy is conducted in two stages. In the initial operation, the front two-thirds of the corpus callosum is severed while preserving the back section, allowing continued sharing of visual information between hemispheres. If this initial intervention fails to control severe seizures, the remaining corpus callosum can be divided during a subsequent procedure. After the corpus callosum is cut, the dura and bone are repositioned, and the scalp is closed using sutures or staples.
Post-Operative Recovery and Continuing Care
Following corpus callosotomy, patients typically remain in the hospital for a duration of two to four days. Most individuals who have undergone this surgery can expect to resume their regular activities, including work or school, within six to eight weeks. Over time, the hair surrounding the surgical incision will regrow, concealing the scar. Importantly, patients will continue taking antiseizure medications to manage their condition in the post-operative phase.
Effectiveness of Corpus Callosotomy
The effectiveness of a corpus callosotomy can be profound, particularly in curbing specific types of seizures. It is most successful in preventing drop attacks, characterized by sudden loss of muscle tone leading to falls, with success rates ranging between 50% to 75%. By minimizing the occurrence of these seizures, corpus callosotomy can substantially reduce the risk of injury and enhance an individual’s overall quality of life.
Side Effects of Corpus Callosotomy
While corpus callosotomy is an effective intervention, it can entail some temporary side effects, which usually resolve over time. These side effects may include:
- Scalp Numbness: A temporary loss of sensation in the scalp near the surgical incision.
- Nausea: Some patients may experience bouts of nausea following the procedure.
- Fatigue and Mood Changes: Feelings of tiredness and mood fluctuations may occur but tend to be transient.
- Headaches: Headaches are a common post-operative symptom.
- Cognitive Effects: Corpus callosotomy can lead to temporary difficulties in speaking, memory, and word retrieval.
- Motor Effects: Some individuals may experience temporary paralysis, weakness, or loss of sensation.
- Personality Changes: Alterations in personality or behavior can manifest as a result of the procedure.
Risks Associated with Corpus Callosotomy
While corpus callosotomy is generally considered a safe procedure, as with any surgery, there are inherent risks. These include:
- Surgical Risks: These encompass potential complications such as infection, bleeding, and rare allergic reactions to anesthesia.
- Brain Swelling: Swelling in the brain can occur post-surgery, necessitating monitoring and intervention.
- Unilateral Awareness: In some cases, there may be a lack of awareness on one side of the body.
- Coordination Issues: Loss of coordination or motor difficulties may be experienced.
- Speech Problems: Stuttering or other speech-related problems can transpire.
- Increase in Partial Seizures: Although the surgery aims to reduce seizures, there is a chance that it might increase the occurrence of partial seizures on one side of the brain.
- Stroke: While infrequent, a stroke is a potential but rare risk associated with this procedure.
In conclusion, corpus callosotomy, a remarkable surgical intervention in the realm of neurosurgery, is specifically designed to alleviate the most severe and intractable forms of epilepsy that have a profound impact on an individual’s daily life. It offers hope and a renewed chance at a higher quality of life to individuals who have faced years of suffering, especially when conventional treatments have proven ineffective in managing their condition. While the procedure is not without its unique set of challenges and potential side effects, its remarkable effectiveness in reducing specific types of seizures and the resultant improvements in cognitive, emotional, and physical well-being make it an invaluable therapeutic option for many who have exhausted other alternatives. As with any intricate medical procedure, a comprehensive and thorough evaluation of both the associated risks and potential benefits is essential. Additionally, meticulous and attentive post-operative care is of paramount importance, ensuring that patients embark on this life-altering journey with the utmost support and guidance from their medical teams.