Infection
3D Printed Materials Could Reduce Infections after Joint Replacements
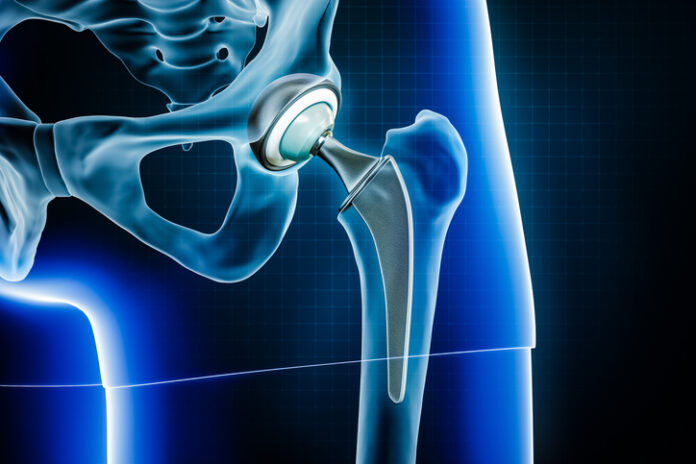
Research led by Washington State University shows a new 3D printed material could help reduce infections linked to medical implants such as knee and hip joint replacements in the future.
As reported in the International Journal of Extreme Manufacturing, the researchers added a small amount of a corrosion-resistant metal called tantalum and copper to a titanium alloy, which is the material commonly used to make joint replacements and other implants.
Although great care is taken to reduce infection risk during joint replacement surgery, a small (one to two percent) but significant number of patients develop an infection at the site of the surgery due to bacterial colonization of the implant, which can be very serious and cause the new joint to fail. These infections often recur on repeat surgery.
“Infection is a problem for which we do not have a solution,” said lead author Amit Bandyopadhyay, Boeing Distinguished Professor in WSU’s School of Mechanical and Materials Engineering, in a press statement.
“In most cases, the implant has no defensive power from the infection. We need to find something where the device material itself offers some inherent resistance—more than just providing drug-based infection control. Here we’re saying, why not change the material itself and have inherent antibacterial response from the material itself?”
In this experimental study, Bandyopadhyay and colleagues used 3D printing technology to make a material combining titanium alloy with 10% tantalum and 3% copper. The copper acts to rupture bacterial cell walls on contact, whereas the tantalum acts to encourage healthy cell growth to integrate bone and soft tissue with the implant.
They then assessed whether bacteria that commonly colonize artificial joints, Pseudomonas aeruginosa and Staphylococcus aureus, were able to colonize the new material over 48 hours exposure. They found that 87% of the bacteria died on contact with the material, which had similar strength to existing implant materials.
“The biggest advantage for this type of multifunctional device is that one can use it for infection control as well as for good bone tissue integration,” said co-author Susmita Bose, Westinghouse Distinguished Professor, at WSU. “Because infection is such a big issue in today’s surgical world, if any multifunctional device can do both things, there’s nothing like it.”
It is early days for this research and the investigators need to do more comprehensive testing before it can get to the clinic. For example, they want to try and increase the number of bacteria that die on contact with the material to almost 100%. However, the results are promising.
The authors write that they think the material “could only improve patients’ postoperative quality of life and reduce revisional surgeries that arise from multiple scenarios, including bacterial infection.”