Infection
Nomogram models to help clinicians predict CRKP infections
Introduction
Bacterial resistance has emerged as a significant challenge in the field of global public health. Klebsiella pneumoniae (KP) is an opportunistic pathogen and one of the common causative agents of community-acquired and healthcare-associated infections. Carbapenem antibiotics are often the drug of last resort when controlling KP infections, but due to widespread use in recent years, CRKP have gradually emerged and become widely prevalent. Compared with carbapenem-sensitive Klebsiella pneumoniae (CSKP), CRKP has garnered more attention from the international community due to its rapid spread and limited treatment options. A multinational prospective cohort study conducted by Wang et al revealed that the 30-day all-cause mortality rate for healthcare-associated CRKP infections is estimated to be 34%, although the characteristics of CRKP infections epidemics vary across regions.1 Genome sequence analysis of 21,016 CRKP strains in 105 countries from 1980 to 2022 in the National Center for Biotechnology Information GenBank database by Yu-Ye Wu et al showed that worldwide, the prevalence of CRKP has progressed from 0.50% prior to 2010 to 31.43% in 2019, and that 51–68% of CRKP strains carry high virulence genes and urgently require increased clinical attention.2 Moreover, according to the 2023 data report from the China Bacterial Resistance Monitoring Network (CHINET), the resistance rates of KP to imipenem and meropenem have escalated rapidly from 3.0% and 2.9% in 2005 to 29% and 30% in 2023.3 The top five provinces in China with the highest CRKP prevalence rates are Henan Province (61.8%), Shanxi Province (58.3%), Beijing City (55.7%), Zhejiang Province (53.3%), and Hebei Province (38%). Our institution, located in the second place, faces a severe situation regarding bacterial resistance.
Although CRKP is increasingly becoming an important problem, the independent contribution of carbapenem resistance and other risk factors to the prediction of CRKP infections is unclear. A number of previous studies have examined risk factors for CRKP infections, but the results were mostly variable and did not lead to consistent conclusions.4–6 Moreover, many of the investigated studies had limited sample sizes or focused on an important department or population, which may confuse the correct perception of CRKP infections among clinical healthcare professionals. In fact, CRKP infections can be widely distributed among various populations. Therefore, a large-scale case-control study to elucidate the predictors of CRKP infections and produce a prediction tool is necessary, which has an important role in early proactive screening for CRKP infections and preventive control by healthcare workers.
Materials and Methods
Study Design
The study was conducted at the 2700-bed Second Hospital of Shanxi Medical University, a regional general medical institution in China. The hospital is located in Taiyuan City, Shanxi Province, an underdeveloped region in central China, and is a Class IIIA general hospital. Patients with KP infections in this institution over a five-year period from January 2018 to January 2023 were included in this study, and the inclusion criteria were: laboratory test specimens were positive for KP and met the Centers for Disease Control and Prevention (CDC) criteria for healthcare-associated infections. Exclusion criteria were: information with missing key data; patients with co-infections with other bacterial infections; and strains identified by the laboratory as non-pathogenic (colonising bacteria). Also, the records of patients with recurrent infections we recorded only once.
The following clinical data were collected from our hospital infection management system “Blue Dragonfly”: (1) the source of the specimen and the department that sent the specimen for examination; (2) the general characteristics of the patient: gender, age, and the duration of the current hospitalisation. (3) Main disease diagnosis: tumour, diabetes, cerebrovascular disease, renal failure, respiratory failure, trauma. (4) Exposure of this hospitalisation: admission to ICU, surgery, central venous catheterisation time, mechanical ventilation time, catheter retention time, days of fever, drain use, blood purification, paracentesis, chemotherapy. (5) Drugs used in this hospitalisation: immunosuppressants, carbapenems, aminoglycosides, cephalosporins, quinolones, tetracyclines, glycopeptides, and β-lactamase inhibitor combination preparations.
Parameter Definition
The following terms were defined prior to analysis:
CRKP infections were defined as KP with a minimum inhibitory concentration of ≥2 mg/L for ertapenem, ≥4 mg/L for imipenem or meropenem, or containing the carbapenemase genes listed above, in accordance with the CLSI Guidelines (29th edition).7 Healthcare-associated infections: hospital-acquired infections in hospitalised patients, including infections acquired during hospitalisation and infections that occur after discharge from hospital acquired in hospital; but excluding infections that have started prior to admission or are in the incubation phase at the time of admission. Infections acquired by hospital staff within the hospital are also hospital-acquired infections.8 Bacterial colonization: a phenomenon in which microorganisms, such as bacteria, grow on a patient’s skin, gastrointestinal tract, respiratory tract, oral cavity, and reproductive tract but have not yet caused clinical manifestations of the associated infection.9
Identification and Drug Sensitivity Analysis of Pathogens
The strains were identified and tested for drug sensitivity based on the VITEK-2 Compact fully automated microbial identification analyser and drug sensitivity analyser (Bio Merieux, France), and the criteria for judging the drug sensitivity results of ertapenem, imipenem, and meropenem were strictly in accordance with the criteria of the American Society for Clinical and Laboratory Standardization (CLSI), and any one of the following criteria was satisfied: minimum inhibitory concentration (MIC) ≥4 μg/mL for imipenem, MIC ≥4 μg/mL for meropenem, and MIC ≥2 μg/mL for ertapenem.7 (The results of drug sensitivity tests were provided by the Microbiology Laboratory of the Second Hospital of Shanxi Medical University).
Statistical Analysis
Preliminary statistical analyses were conducted using SPSS 26.0 software. The Shapiro–Wilk normality test was used to determine the normality of the quantitative data. If the data followed a normal distribution, they were expressed as (x±s) and independent samples t-test were used for between-group comparisons. If the data were not normally distributed, they were expressed as M(P25, P75) and Wilcoxon rank-sum tests were used for between-group comparisons. Count data were described using frequency (%) and comparisons between groups were made using the Chi-square test or Fisher’s exact probability method. Statistical significance was considered at p<0.05. The analyses were visualized using R (4.3.1) software. The dataset was randomly selected 275 cases as the training set and the remaining 118 cases as the validation set (0.7: 0.3) without missing values. Using the data from the training set, the cv.glmnet function cross-validation was applied to build the LASSO prediction model, and the number of cross-validations was set to 10.10 Logistic regression was performed on the screened variables and the results were presented in nomogram model. ROC curves and calibration curves were also plotted to assess the predictive value of the nomogram model for CRKP infections.
Results
Patient Characteristics
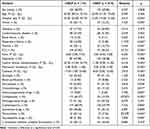
Between January 2018 and January 2023, a total of 4954 patients were diagnosed with Klebsiella pneumoniae infections. Of these, 4561 were excluded because they met the exclusion criteria, and the patient inclusion flow chart is shown in Figure 1. 393 infections were finally included in the analysis, with CRKP occurring in 174 cases (44.3%) and CSKP in 219 cases (55.7%). The age range of patients is 15–97 years old, with an average age of 62 years. The majority are male (273 cases, 67.47%). Overall, the most common primary diagnoses were cerebrovascular-related diseases (116 cases, 29.5%), diabetes mellitus (74 cases, 18.8%), and malignancy (62 cases, 15.8%). The main antimicrobials exposed before specimen culture were cephalosporins (239, 60.8%), carbapenems (142, 36.1%) and quinolones (161, 40.9%). Table 1 shows all clinical and demographic characteristics of patients with Klebsiella pneumoniae infections. The two groups were compared in terms of length of hospital stay, malignancy, respiratory failure, trauma, ICU admission, days of fever, central venous catheterisation, mechanical ventilation, urinary catheterisation, paracentesis, chemotherapy, use of immunosuppressants, carbapenems, cephalosporins, quinolones, tetracyclines, and glycopeptides (p < 0.05).
|
Table 1 Demographic and Clinical Characteristics of Patients with KP Infection |
|
Figure 1 KP infection case screening flow chart. |
In addition, Table 2 summarizes the departmental distribution of the 174 CRKP patients, in which the ICU constituted the highest ratio (60, 34.4%), neurosurgery and haematology constituted the higher ratios (25 and 41, 14.3% and 25.3%), and the rest of the departmental infections were basically evenly distributed. Table 3 summarizes the types of specimens.
|
Table 2 Department Distribution of 174 CRKP Patients |
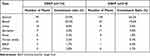 |
Table 3 Composition Ratio of Cultivated Specimens |
At our institution, CRKP was isolated more frequently from respiratory cultures compared to samples of blood, urine or intestinal origin, which essentially mirrors our microbiological surveillance pattern. Of the 174 bacterial strains, sputum specimens accounted for 93 strains (53.4%), blood specimens for 41 strains (23.5%), urine specimens for 15 strains (8.6%), and faecal or rectal swabs for a low percentage of 6 strains (3.4%). This indicates that we are not standardised enough in retaining culture specimens for CRKP infections. Sterile body fluids (blood, bone marrow, cerebrospinal fluid, etc.) and correctly taken urine specimens are of high diagnostic value, whereas sputum culture specimens have limited diagnostic value due to their high possibility of contamination. The correct microbiological culture pattern in healthcare facilities should be based on sterile specimens.11 From 2018 to 2023, we are still trying our best to standardise the collection and delivery of microbiological specimens and to increase the proportion of microbiological specimens collected from sterile sites that are delivered for testing, because the correct diagnosis and treatment of infectious diseases need to be based on correct microbiological testing.
Infection Prediction Model Based on Lasso-Logistic Regression
All variables from the baseline data were included in the LASSO regression model, and the quantitative variables were recorded as actual values, categorical variables were assigned values, and the assignment rules were as follows: male = 1, female = 2; suffering from (tumour, diabetes mellitus, cerebrovascular disease, renal failure, respiratory failure, trauma) = 1, none = 0; having (admission to the ICU, surgery, drainage tubes, haemodialysis, body puncture surgery, chemotherapy) = 1, none = 0; using (Immunosuppressive drugs, carbapenems, aminoglycosides, cephalosporins, quinolones, tetracyclines, glycopeptides, β-lactamase inhibitor combinations) = 1, none = 0. LASSO cross-validation plots (Figure 2) and regression path diagrams were constructed (Figure 3). Six predictors were screened for admission to and stay in the ICU, duration of fever, duration of central venous catheterisation, duration of catheter retention, carbapenem use, and tetracycline use. The logistic regression results are shown in Table 4.
 |
Table 4 Results of Logistic Multiple Factor Regression Analysis |
|
Figure 2 LASSO Cross validation diagram. |
|
Figure 3 LASSO regression path diagram. |
The prediction model containing the above 6 predictors was presented in the form of a more intuitive nomogram model (Figure 4), which facilitates healthcare professionals to perform active CRKP risk screening in advance. The discrimination and calibration of the prediction models were assessed by ROC curves and calibration curves. The area under the ROC curve (AUC) value was 0.894 (95% CI: 0.857, 0.931) for the training set (Figure 5) and 0.872 (95% CI: 0.805, 0.939) for the validation set (Figure 6), and the results of the two showed that the model had a high diagnostic value. The calibration curve (Figures 7 and 8) shows the predicted CRKP risk incidence on the X-axis and the actual CRKP risk incidence on the Y-axis. The dashed diagonal line in the figure represents the ideal state, and the solid line represents the columnar graphical model of this study; the closer the fit to the diagonal dashed line, the better the prediction. The figure shows that the two are basically close to each other, with good prediction accuracy between the actual and predicted probabilities.
|
Figure 4 A Nomogram Model for Predicting CRKP Infection. |
|
Figure 5 ROC curve of training sets. |
|
Figure 6 ROC curve of validation sets. |
|
Figure 7 Calibration curve of training sets. |
|
Figure 8 Calibration curve of validation sets. |
Discussion
The incidence of CRKP infections is increasing year by year, and has become a major threat to global public health security. CRKP are resistant to antibiotics through a variety of mechanisms, including carbapenemase-producing enzymes, which efficiently hydrolyse cephalosporins and carbapenems, rendering treatment ineffective; deletion or down-regulation of bacterial outer membrane proteins, which results in the inability of antibiotics to enter the bacterium through the cell membrane, leading to the excessive production of ultra-broad-spectrum β-lactamases (ESBLs); overexpression of genes encoding the exocytosis pumps, which results in the increased clearance of antibacterial drugs; structural changes in penicillin-binding proteins, leading to a decrease in their affinity for carbapenems. Among them, carbapenemase-producing enzymes are the most predominant mechanism in our country.12,13 In China, the most prevalent carbapenemase is KPC-2 (Klebsiella pneumoniae carbapenemases), which accounts for more than 70% of CRKP enzymes in China, and patients with CRKP infections carrying KPC-2 enzymes have higher levels of drug resistance. In conclusion, early identification of CRKP-infected patients is urgently needed to improve their survival outcomes in clinical practice. In this study, we successfully constructed a nomogram model for predicting the probability of developing CRKP infection, which can be used as a tool for healthcare professionals to screen for infections at an early stage, which may help to improve the prognosis of patients.
In this study, we analysed the data of KP patients with Healthcare-associated infections in a hospital in China through a retrospective case-control and cohort study, and established a nomogram model based on several variables screened by Lasso regression. The model developed involves six clinically used indicators, which are admission to ICU, duration of fever, duration of central venous catheterisation, duration of indwelling urinary catheter, carbapenem use, and tetracycline use. The above indicators can be used to comprehensively assess an individual’s risk of infection and thus well predict the occurrence of infection. Previous studies have found that haemodialysis14 and renal failure15 may also be independent risk factors for CRKP infection. However, the present study did not yield these results, which may be due to regional differences in the location of healthcare facilities and lack of sample size.
In this study, admission to ICU and invasive procedures such as central venous catheterisation and indwelling urinary catheter were found to be risk factors for the development of CRKP infection. Patients admitted to ICUs often have rapidly changing conditions and inevitably require a variety of invasive operations to urgently maintain life. Intubation or tracheostomy easily damages normal body tissues and reduces the immunity of patients, and opportunistic pathogens are more likely to invade and attach to the inner wall of the respiratory tract, forming a biofilm cover, which undoubtedly increases the risk of Klebsiella pneumoniae turning from colonisation to infection and from mild to severe disease in ICU patients. Therefore, it is all the more important to strengthen the ICU medical staff’s understanding of the degree of sensory control associated with invasive devices/operations, to master the indications for the use of various invasive devices and tubes, and to make a good daily assessment, so as to avoid the unnecessary use of and redundancy in the retention of various tubes and tubes.
The empirical use of carbapenems as an independent risk factor for CRKP infection is not controversial and does not need to be described here. Most importantly, it has been noted that the empirical use of tetracyclines such as tigecycline and doxycycline is also an independent risk factor for CRKP infection, which is consistent with the results of this study.16 In recent years, high levels of tigecycline resistance have emerged due to bacterial variation and poor drug use, and because of tigecycline’s own pharmacokinetic limitations (low concentrations in blood and cerebrospinal fluid) and its low bacteriostatic properties at low concentrations. Currently, two- or three-drug combinations are generally recommended, often in combination with polymyxins, carbapenems, and aminoglycosides. A meta-analysis showed that tigecycline combination therapy for CRKP infections had a lower morbidity and mortality rate than its monotherapy.17 In recent years, several β-lactamase inhibitor combinations have been used in our country, and ceftazidime/avibactam and imipenem-cilastatin are commonly used in our region, because both of them have strong antimicrobial activity against multidrug-resistant Gram-negative bacilli, including KPC enzyme-producing ones. We expected to go to the conclusion of the predictive value of such drugs for the diagnosis of CRKP infections, but we came up with nonsignificant results.
Limitation of the Study
The present study is a single-centre retrospective study, and multi-regional, prospective studies are still needed to further explore this. Limitations also include the following: first, we only extracted data from patients with positive samples for the first test and did not take into account secondary infections, multiple culture results, and so on. Second, the variable of drug combination therapy was not included in this study because of the difficulty in finding the history of drug combination therapy from past information. Third, we did not include the factor of Klebsiella pneumoniae colonisation as a variable. Due to financial constraints and other reasons, active screening was not widely implemented for all patients at admission, so we may not have been accurate about bacterial colonisation. In reality, however, bacterial colonisation and bacterial infection are undoubtedly correlated and should be treated as an important factor.
Conclusion
In conclusion, the risk prediction model developed in this study allows for individualised prediction of high-risk patients so that diagnostic and therapeutic strategies can be targeted to reduce the incidence of CRKP infections.
Ethics Approval and Consent to Participate
The study was approved by the Ethical Review Committee of the Second Hospital of Shanxi Medical University, which waived the requirement for informed consent due to the type of retrospective study and the anonymity of patient information/records (no.2022YX020). This study was in compliance with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for the contents of the work.
Funding
We received funding from the General Soft Science Program of Shanxi Province, China. Fund No. 2017041037-2.
Disclosure
All authors declare that there are no conflicts of interest in this article.
References
1. Wang M, Earley M, Chen L, et al. Clinical outcomes and bacterial characteristics of carbapenem-resistant Klebsiella pneumoniae complex among patients from different global regions (CRACKLE-2): a prospective, multicentre, cohort study. Lancet. 2022;22(3):401–412. doi:10.1016/S1473-3099(21)00399-6
2. Wu Y, Wu C, Bao D, et al. Global evolution and geographic diversity of hypervirulent carbapenem-resistant Klebsiella pneumoniae. Lancet Infect Dis. 2022;22(6):761–762. doi:10.1016/S1473-3099(22)00275-4
3. Changes of drug resistance of Klebsiella pneumoniae to imipenem and meropenem. Institute of antibiotics, Huashan Hospital, Fudan University, China. Available from: http://www.chinets.com/Data/GermYear. Accessed September 9, 2023.
4. Lou T, Du X, Zhang P, et al. Risk factors for infection and mortality caused by carbapenem-resistant Klebsiella pneumoniae: a large multicentre case-control and cohort study. J Infect. 2022;84(5):637–647. doi:10.1016/j.jinf.2022.03.010
5. Çölkesen F, Tarakçı A, Eroğlu E, et al. Carbapenem-resistant Klebsiella pneumoniae infection and its risk factors in older adult patients. Clin Interv Aging. 2023;18:1037–1045. doi:10.2147/CIA.S406214
6. Candevir Ulu A, Kurtaran B, Inal AS, et al. Risk factors of carbapenem-resistant Klebsiella pneumoniae infection: a serious threat in ICUs. Med Sci Monit. 2015;21:219–224. doi:10.12659/MSM.892516
7. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Thirty-First Informational Supplement. Wayne PA: CLSI; 2021.
8. Hospital infection surveillance standards. National Health Commission of the People’s Republic of China. Available from: http://www.nhc.gov.cn/wjw/s9496/202309/432d0f9af63443e890019af57afaf853.shtml. Accessed September 9, 2023.
9. Chinese Expert Consensus on Diagnosis, Treatment, Prevention and Control of Carbapenem-Resistant Enterobacteriaceae Bacterial Infections, China Medical Education Association Infectious Diseases Committee, Chinese Medical Association Bacterial Infections and Drug-Resistant Infections Prevention and Control Committee. Expert consensus on diagnosis, treatment, prevention and control of carbapenem-resistant Enterobacteriaceae bacterial infections in China. Chinese Med J. 2021;101(36):2850–2860. doi:10.3760/cma.j.cn112137-20210219-00438.
10. Kidd AC, McGettrick M, Tsim S, et al. Survival prediction in mesothelioma using a scalable Lasso regression model: instructions for use and initial performance using clinical predictors. BMJ Open Respir Res. 2018;5(1):e000240. doi:10.1136/bmjresp-2017-000240
11. Guidelines for the prevention and control of carbapenem-resistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in health care facilities. World Health Organization; 2017. Available from: https://www.who.int/publications/i/item/9789241550178. Accessed November 27, 2023.
12. Wang YP, Chen YH, Hung IC, et al. Transporter genes and fosa associated with fosfomycin resistance in carbapenem-resistant Klebsiella pneumoniae. Front Microbiol. 2022;13:816806. doi:10.3389/fmicb.2022.816806
13. Yang J, Zhang K, Ding C, Wang S, Wu W, Liu X. Exploring multidrug-resistant Klebsiella pneumoniae antimicrobial resistance mechanisms through whole genome sequencing analysis. BMC Microbiol. 2023;23(1):245. doi:10.1186/s12866-023-02974-y
14. Zhou S, Ren G, Liu Y, et al. Challenge of evolving Klebsiella pneumoniae infection in patients on hemodialysis: from the classic strain to the carbapenem-resistant hypervirulent one. Int J Med Sci. 2022;19(3):416–424. doi:10.7150/ijms.69577
15. Zhang F, Zhong J, Ding H, et al. Analysis of risk factors for carbapenem-resistant Klebsiella pneumoniae infection and its effect on the outcome of early infection after kidney transplantation. Front Cell Infect Microbiol. 2021;11:726282. doi:10.3389/fcimb.2021.726282
16. Yu R, Li L, Zou C, et al. Emergence of high-level tigecycline resistance due to the amplification of a tet(A) gene variant in clinical carbapenem-resistant Klebsiella pneumoniae. Clin Microbiol Infect. 2023;29(11):1452–e1. doi:10.1016/j.cmi.2023.07.030
17. Ni W, Han Y, Liu J, et al. Tigecycline treatment for carbapenem-resistant Enterobacteriaceae infections: a systematic review and meta-analysis. Medicine. 2016;95(11):e3126. doi:10.1097/MD.0000000000003126