Cancer
When and How Should You be Screened for Colon Cancer?
Colon cancer, being the second-deadliest form of cancer after lung cancer, has recently seen updates in guidance for screening, leading to some confusion. In August, the American College of Physicians (ACP) released new recommendations that diverge from those of other major organizations, such as the American Cancer Society (ACS) and the US Preventive Services Task Force (USPSTF).
So, what do you need to know?
How does the advice differ?
It’s crucial to highlight that the advice provided pertains specifically to individuals at average risk without a family history of colon cancer. If you have a family history or other factors that elevate your risk for colorectal cancer, it’s essential to consult with your doctor to determine the most appropriate course of action for your specific situation.
The primary point of contention revolves around the age at which individuals should commence screening. The recent guidance from the ACP advocates for starting screening at age 50, whereas the ACS and USPSTF recommend initiating screening at age 45. The U.S. Multisociety Task Force on Colorectal Cancer aligns with the recommendation to begin screening at age 45. This perspective is also supported by numerous physicians, including Dr. Andrew T. Chan, a gastroenterologist and director of epidemiology at Massachusetts General Hospital Cancer Center, who is a professor at Harvard Medical School. Dr. Chan provides further clarification on key facts related to this topic.
Why do experts suggest starting screening earlier?
Dr. Chan highlights a concerning and unexplained increase in the incidence of colon cancer in individuals younger than 50. While overall deaths from colon cancer exhibited a 2% per year decline from 2011 to 2020, the trend is starkly different for those under 50. In this age group, deaths from colon cancer rose between 0.5% and 3% during the same period, as reported in 2023 statistics.
This rise in colon cancer rates among younger individuals is observed across all racial and ethnic groups, with particularly notable increases among Alaskan Natives and Native Americans. Overall, Blacks and African Americans have a higher likelihood of both contracting and succumbing to colon cancer than whites, and early-onset cases are more prevalent in Black individuals compared to whites.
The initiative to promote colon cancer screening began in the mid-1990s, and approximately 60% of adults over 50 currently adhere to the recommendation for regular colonoscopies. While this compliance has likely contributed to the decline in deaths from colon cancer in older adults, Dr. Chan emphasizes the need for earlier screening to curb the rising incidence of early-onset cases, particularly for individuals in their 40s. Additionally, there is evidence suggesting that earlier colonoscopies may be associated with a reduced incidence of colon cancer even later in life.
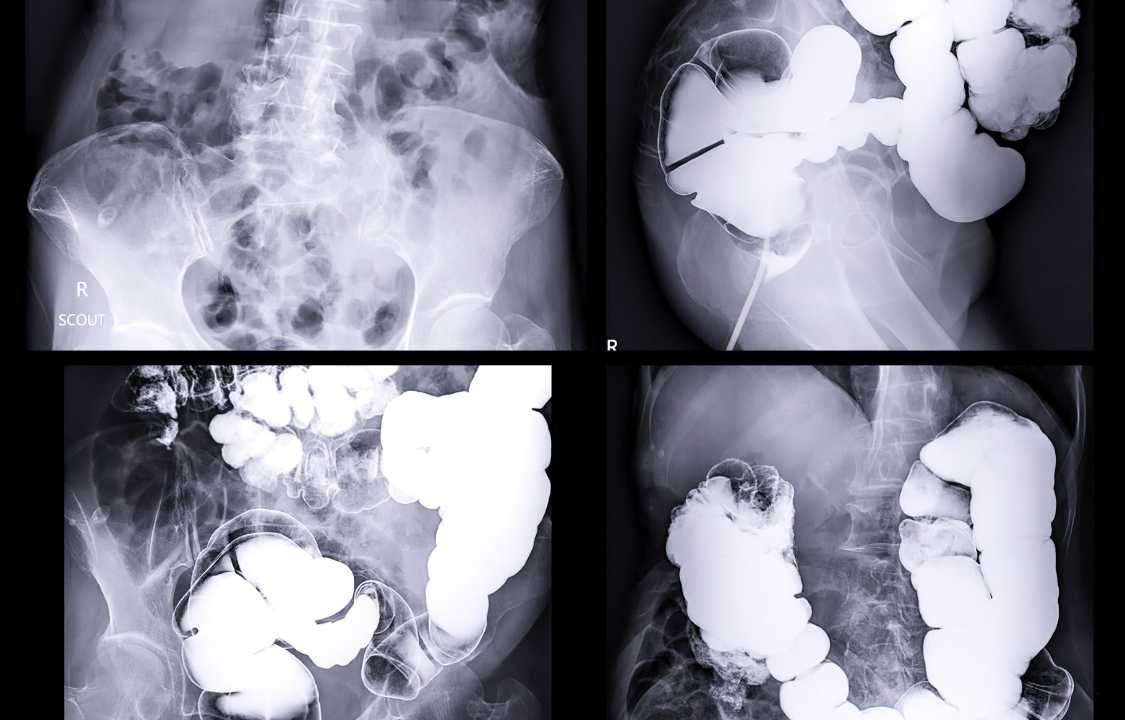
What are the different screening tests for colon cancer?
The two primary screening tests for colon cancer are the standard colonoscopy and various stool-based tests:
1. Colonoscopy:
- Procedure: A gastroenterologist or surgeon uses a long, flexible tube with a camera to examine the entire length of the colon.
- Detection: It is considered the gold-standard test, capable of identifying precancerous polyps (adenomas) and facilitating their removal during the procedure.
- Preparation: Requires taking laxatives and drinking fluids to cleanse the colon.
- Complications: Serious complications like perforation or bleeding are rare, occurring in about three in 1,000 procedures.
- Frequency: If no polyps are found, a repeat colonoscopy is generally recommended every 10 years. If polyps are present or there is a change in risk or symptoms, the interval may be shorter.
2. Stool Tests:
Fecal Occult Blood Test (FOBT) and Fecal Immunochemical Test (FIT):
- Detection: These tests check for blood in small stool samples collected at home.
- Frequency: Recommended annually.
FIT-DNA Test:
- Detection: Checks for both blood and abnormal DNA in stool samples.
- Frequency: Typically repeated every three years.
Additionally, the American College of Physicians suggests another option:
Flexible Sigmoidoscopy:
- Procedure: Inspects only the lower part of the colon.
- Frequency: Recommended once every 10 years, combined with fecal FIT testing every two years (although sigmoidoscopy is rarely ordered in the United States today).
If flexible sigmoidoscopy or any stool tests indicate a potential issue, a colonoscopy is typically recommended to further investigate and check for adenomas or cancer. The choice of screening method depends on various factors, including individual risk, preferences, and medical history. Regular screening is essential for early detection and prevention of colon cancer.
Why might stool-based screening make sense for younger adults?
Dr. Chan emphasizes that a colonoscopy may not be the optimal initial screening test for everyone, especially for younger individuals, primarily due to its time-consuming and inconvenient nature.
“If you find it challenging to make time in your schedule or have concerns about undergoing a colonoscopy,” he notes, “a stool-based test, which is noninvasive and requires very little time, is a suitable alternative.”
Dr. Chan underscores the importance of taking action, stating that not doing anything is the least favorable option. Early detection and treatment are crucial for preventing deaths related to colon cancer. Choosing a screening method that aligns with individual preferences, schedule constraints, and concerns is essential, as regular screening remains a key component in the prevention and early intervention of colon cancer.