Insight, Medical Care
Understanding Osteoporosis — the Basics
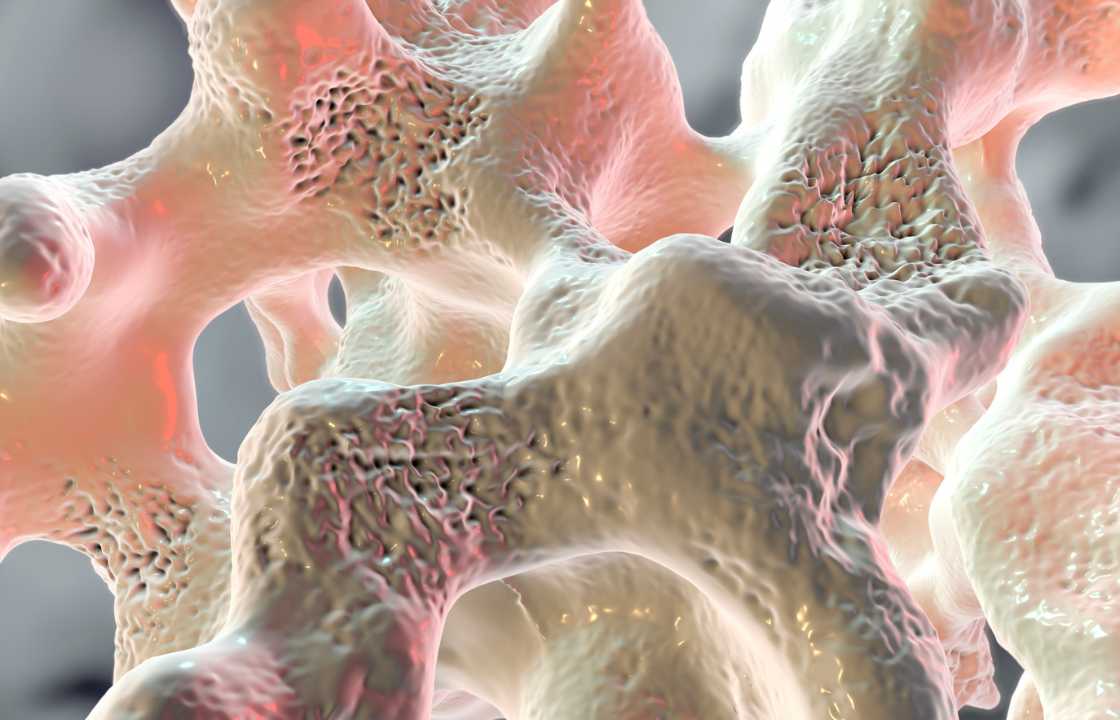
Osteoporosis, often referred to as “porous bones,” is a silent but potentially debilitating condition that gradually weakens bones, increasing the risk of fractures. In the United States alone, an estimated 2 million fractures each year can be attributed to osteoporosis.
While osteoporosis can affect any bone in the body, fractures of the spine, hip, and wrist are most common. In older individuals, hip fractures can be particularly perilous, often resulting in prolonged periods of immobility during the healing process, which can lead to potentially life-threatening complications like blood clots or pneumonia.
Of the approximately 10 million Americans living with osteoporosis, a staggering 80% are women. This gender disparity is largely attributed to the fact that women typically have lighter and less dense bones and undergo significant hormonal changes post-menopause, which accelerate the loss of bone mass.
Understanding the Causes of Osteoporosis
The human body continuously undergoes a process called bone remodeling, where old bone is broken down and replaced with new bone. Bone mass typically reaches its peak in a person’s mid to late 20s.
Bone loss, where the rate of bone breakdown exceeds the rate of bone buildup, typically commences in the mid-30s. As individuals age, bones start losing calcium – the mineral responsible for bone hardness – faster than they can replenish it. This results in a reduction in bone remodeling and a gradual thinning of bones.
In women, bone density loss accelerates during the first 5 to 7 years following menopause and subsequently decelerates. Scientists attribute this to a sharp decline in the body’s production of estrogen, a hormone that helps maintain calcium in bones.
While some degree of bone density loss is a natural part of the aging process, certain factors increase the risk of developing severe bone fragility and fractures associated with osteoporosis. These risk factors include:
- Body Composition: Individuals who are thin or have a small frame are at a higher risk.
- Lifestyle Choices: Habits such as smoking, excessive alcohol consumption, and a sedentary lifestyle are associated with an increased risk of osteoporosis.
- Family History: A family history of hip fractures can elevate an individual’s risk.
- Ovarian Removal: Having one’s ovaries removed, especially before the age of 40, can increase the risk.
- Ethnicity: Individuals of white or Asian ethnicity are more susceptible.
- Medical Conditions: Certain medical conditions that enhance bone breakdown, such as kidney disease, Cushing’s syndrome, an overactive thyroid or parathyroid, can lead to osteoporosis. The prolonged use of glucocorticoids (steroids) and immobility due to paralysis or illness can also result in bone loss.
The Role of Lifestyle Habits in Bone Health
Daily habits significantly impact bone health. Proper nutrition and physical activity play pivotal roles in preventing and managing osteoporosis.
- Vitamin D and Calcium: Adequate intake of vitamin D and calcium is essential for strong bones. The National Institutes of Health recommends 600 IU of vitamin D daily for adults up to 70 years of age, increasing to 800 IU for those over 70. Both men up to age 70 and women up to age 50 require 1000 mg of calcium daily, with men over 70 and women over 50 needing 1200 mg daily.
- Fruits and Vegetables: A diet rich in fruits and vegetables provides magnesium, potassium, and vitamin K, all of which contribute to bone health.
- Protein: While sufficient protein intake is crucial for bone health, excessive consumption of nondairy animal protein can weaken bones. Consult with your healthcare provider for personalized protein recommendations.
- Caffeine: Excessive caffeine intake can negatively affect bone health.
- Alcohol: Excessive alcohol consumption can decrease bone formation and is associated with an increased risk of falls, particularly in older individuals.
- Physical Activity: Engaging in regular physical activity, including weight-bearing exercises like brisk walking and muscle-strengthening activities, helps maintain strong bones.
- Smoking: Studies have shown that smoking has detrimental effects on bone health.
Diagnosis and Testing for Osteoporosis
To diagnose osteoporosis, healthcare providers typically perform a comprehensive evaluation, which may include a medical history assessment, bone density testing, and additional diagnostic procedures.
During an examination, the healthcare provider will:
- Consider your age, menopausal status in women, previous adult fractures, family history, and lifestyle factors like smoking, alcohol consumption, and physical activity.
- Review any medications you are taking, as some drugs, such as corticosteroids, can lead to bone weakening with prolonged use.
- Conduct a physical examination, including assessing your height and inspecting your spine for any abnormal curvatures, which can indicate previous spinal fractures associated with osteoporosis.
Bone Density Testing: Bone density testing is a noninvasive procedure that measures the mineral concentration in the bones of the hip, spine, and sometimes the forearm. These results are compared to established norms to determine whether an individual has low bone density (osteopenia) or full-blown osteoporosis.
Understanding Osteoporosis Treatment
If diagnosed with osteoporosis, healthcare providers will typically recommend prescription drugs aimed at limiting bone breakdown, maintaining bone density, and reducing the risk of osteoporotic fractures, particularly in the hips and spine. Several classes of drugs have been shown to effectively reduce fracture risk. These drugs include:
- Bisphosphonate Drugs: Bisphosphonates such as alendronate (Fosamax), alendronate sodium (Binosto), ibandronate (Boniva), risedronate (Actonel, Atelvia), and zoledronic acid (Reclast, Zometa) are widely used to strengthen bones and lower fracture risk.
Other Medications: Additional medications that protect against bone loss include:
- Raloxifene (Evista): An estrogen-like drug that increases bone density and reduces fracture risk.
- Romosozumab-aqqg (Evenity): An anti-sclerostin antibody that promotes bone formation and reduces bone loss.
- Abaloparatide (Tymlos) and teriparatide (Forteo): Synthetic forms of parathyroid hormone suitable for individuals at high fracture risk. These medications support bone density increase.
- Denosumab (Prolia, Xgeva): An antibody that inhibits the formation of bone-resorbing cells, reducing bone loss.
- Calcitonin: A naturally occurring hormone that aids in fracture prevention and bone loss reduction.
It’s important to communicate all medications you are taking to your healthcare provider, as certain drugs may impact bone health. Your healthcare provider may adjust your medications or recommend alternative treatments.
After using bisphosphonates for five years or more, there is a low risk of developing a thigh bone fracture, and in such cases, transitioning to a different medication may be considered.
- Hormone Replacement Therapy (HRT): Hormone replacement therapy, involving estrogen alone or a combination of estrogen and progestin, can prevent and treat osteoporosis. However, research has demonstrated that HRT increases the risk of breast cancer, heart disease, and stroke in certain women. Therefore, HRT is not typically recommended as the initial treatment for osteoporosis in most women, as the potential health risks often outweigh the benefits. Women who have previously used menopausal hormone therapy and discontinued it may experience a resurgence of bone thinning at a rate comparable to that during menopause.
Recovery After a Fracture
Fractures due to osteoporosis commonly occur in the hip, wrist, and spine. Hip fractures often necessitate surgical intervention, while wrist fractures may require casting or surgery.
Spinal fractures are prevalent among seniors and can lead to chronic back pain and a reduction in height. In some cases, severe pain can result in additional health issues.
Pain Relief Options for Fractures
Pain management for fractures associated with osteoporosis may involve various options:
- Over-the-Counter Pain Relievers: Aspirin or acetaminophen can alleviate mild pain.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Drugs such as ibuprofen and naproxen can reduce pain and swelling but should be used cautiously and under medical guidance.
- Prescription Pain Medications: In cases of severe pain, healthcare providers may prescribe opioid pain medications, like codeine or morphine. However, extended use of these potent medications is discouraged due to potential side effects.
- Physical Therapy: Physical therapy can help individuals learn proper movement techniques to minimize the risk of further fractures.
Two minimally invasive surgical procedures can address back pain related to fractures:
- Kyphoplasty: This procedure involves the insertion of a balloon to expand fractured vertebrae, followed by the injection of bone cement to stabilize the affected area. The balloon is then deflated and withdrawn.
- Vertebroplasty: In this procedure, bone cement is injected directly into the fractured vertebrae.
When considering these surgical options, patients should engage in thorough discussions with their healthcare providers to understand the benefits and potential risks, including cement leakage and side effects like tissue damage, blood clots in the lung, and respiratory failure.
Complications of Osteoporosis Bone Fractures
Fractures resulting from osteoporosis can significantly disrupt daily activities, including bending, descending stairs, and cooking. Timely treatment, physical therapy, and the adoption of a healthy lifestyle can improve the well-being of individuals living with osteoporosis.
In conclusion, osteoporosis is a prevalent condition that primarily affects women and the elderly. However, it is not an inevitable part of aging, and numerous factors, including lifestyle choices and early intervention, can significantly influence an individual’s risk and experience of osteoporosis. Awareness of risk factors, regular bone health assessments, and appropriate treatment are essential to protect bone health and prevent debilitating fractures. By promoting proactive bone health, individuals can maintain an active and fulfilling lifestyle, free from the constraints of osteoporosis.