Disease
Kawasaki Disease
Kawasaki disease, a complex and potentially serious condition, manifests as inflammation in the walls of small to medium-sized blood vessels that traverse the body, with a predilection for impacting the heart arteries in children. Termed mucocutaneous lymph node syndrome, this ailment extends its influence beyond the cardiovascular system, inducing swelling in glands (lymph nodes) and mucous membranes within the oral cavity, nasal passages, eyes, and throat.
Children afflicted by Kawasaki disease often exhibit a constellation of symptoms, including a high fever, swollen hands and feet with skin peeling, and red eyes and tongue. Despite the alarming presentation, the disease is frequently treatable, with early intervention leading to a positive prognosis and minimal long-term complications.
Symptoms encompass a fever exceeding 102.2 degrees Fahrenheit (39 degrees Celsius) persisting for five or more days. To establish a diagnosis, a child must display at least four of the following:
1. A rash on the main part of the body or in the genital area.
2. Enlarged lymph nodes in the neck.
3. Very red eyes without a thick discharge.
4. Red, dry, cracked lips and a red, swollen tongue.
5. Swollen, red skin on the palms of the hands and the soles of the feet, with subsequent peeling of the skin on fingers and toes.
It is noteworthy that these symptoms may not occur simultaneously, emphasizing the importance of communicating with healthcare professionals, even if a symptom appears to have subsided. Additional symptoms may include belly pain, diarrhea, fussiness, joint pain, and vomiting. In some instances, children may experience a prolonged high fever but have fewer than four of the required symptoms for a definitive diagnosis, leading to the classification of incomplete Kawasaki disease. Even in cases of incomplete presentation, prompt treatment within 10 days of symptom onset is crucial to mitigate the risk of heart artery damage.
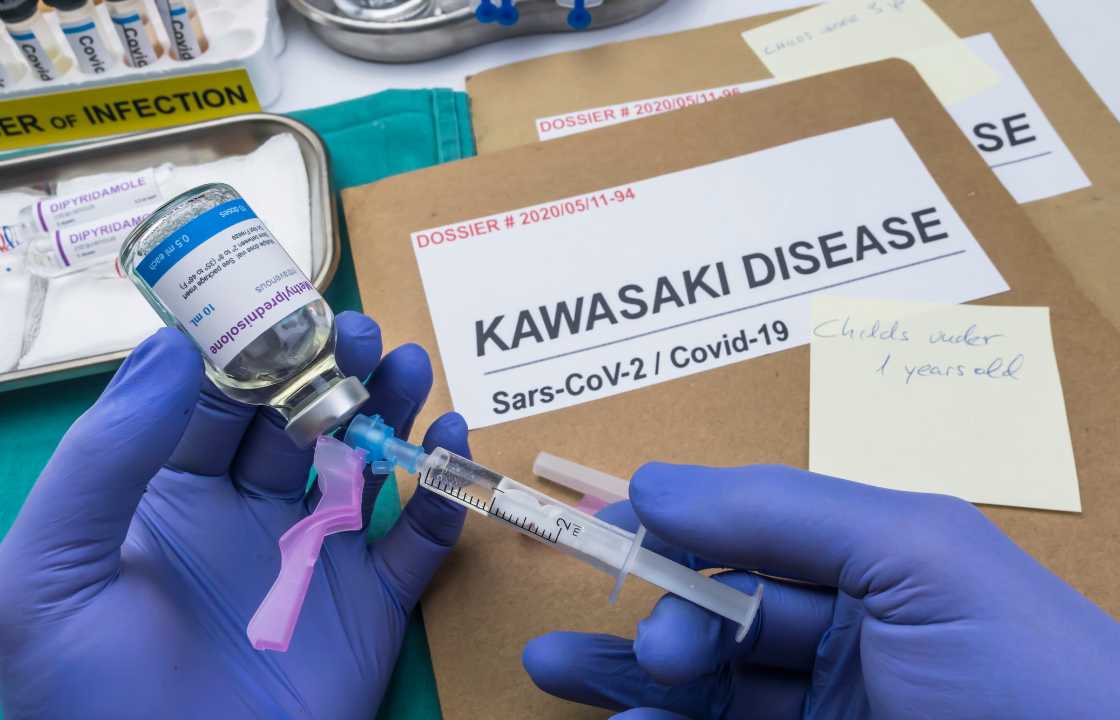
It is imperative to recognize that Kawasaki disease shares clinical features with a condition known as multisystem inflammatory syndrome in children, which arises in the context of COVID-19 infection. Therefore, accurate diagnosis and timely medical attention are critical to distinguish between these conditions.
Parents and caregivers should be vigilant, seeking medical advice if a child experiences a fever lasting more than three days. Early intervention within the first 10 days of symptom onset plays a pivotal role in reducing the likelihood of lasting damage to the heart arteries.
The precise etiology of Kawasaki disease remains elusive, with experts dismissing person-to-person transmission. Proposed theories suggest potential associations with bacterial or viral infections, environmental factors, and genetic predispositions. Specific genes may heighten children’s susceptibility to Kawasaki disease.
Several risk factors contribute to the likelihood of developing Kawasaki disease, including age, with children under 5 years old at the highest risk. Additionally, assigned male children and those of Asian or Pacific Islander descent exhibit a slightly elevated risk. The disease displays a seasonal pattern, often peaking in winter and early spring in regions with climates similar to North America.
Kawasaki disease, despite being a leading cause of heart disease in children in developed countries, is characterized by a favorable prognosis with appropriate treatment. Timely and suitable intervention significantly minimizes the risk of lasting damage. Potential complications include the swelling of blood vessels, particularly the arteries supplying blood to the heart, swelling of the heart muscle, and heart valve problems. These complications can result in heart damage, with arterial swelling potentially leading to aneurysms, increasing the risk of blood clots, heart attacks, or internal bleeding.
In rare instances, children with heart artery complications from Kawasaki disease may face life-threatening consequences. The overall prognosis emphasizes the critical importance of early detection, intervention, and ongoing medical monitoring to ensure the well-being of children affected by this complex and potentially severe condition.
Diagnosing Kawasaki disease involves a comprehensive approach, as there is no single test for its identification. Diagnosis entails ruling out other diseases that manifest similar symptoms, such as scarlet fever, juvenile rheumatoid arthritis, Stevens-Johnson syndrome, toxic shock syndrome, measles, and illnesses caused by ticks, like Rocky Mountain spotted fever. Healthcare professionals conduct a thorough examination, coupled with blood and urine tests, including a complete blood count to assess inflammation.
Additional diagnostic tools include an electrocardiogram (ECG or EKG) to evaluate the heart’s electrical activity and an echocardiogram that employs sound waves to create images of the heart in motion. These tests aid in assessing blood flow, heart valve function, and potential problems with the heart arteries.
Treatment for Kawasaki disease is most effective when initiated early during the fever phase. Typically administered in a hospital setting, the goals of treatment are to lower fever, reduce swelling, and prevent heart damage. Medications employed include gamma globulin, a protein delivered intravenously to lower inflammation in the blood vessels and mitigate the risk of heart artery complications. Aspirin is also utilized in high doses to treat inflammation, alleviate pain, joint swelling, and fever. Post-treatment, low-dose aspirin may be recommended for an extended period, especially if there are concerns about heart artery issues.
For comprehensive care and monitoring, follow-up tests to assess heart health are often conducted 6 to 8 weeks after the onset of illness, with additional evaluations after six months if necessary. Children exhibiting signs of persistent heart problems may be referred to a pediatric cardiologist, who specializes in treating heart disease in children, for further management.
The coping and support aspect of Kawasaki disease involve acquiring in-depth knowledge about the condition to make informed decisions with the healthcare team. Most children treated for Kawasaki disease experience rapid recovery and resume their usual activities. In cases where the heart is affected, consultation with a pediatric cardiologist may guide decisions regarding activity restrictions.
Preparing for a medical appointment involves compiling relevant information, including the child’s symptoms, their duration, improvements or exacerbations, and any potential exposure to infectious diseases. A list of current medications, vitamins, or supplements should also be documented, along with pertinent questions for the healthcare professional.
In conclusion, Kawasaki disease poses a multifaceted challenge, necessitating vigilance, early intervention, and ongoing medical care for optimal outcomes. The collaborative efforts of healthcare professionals, parents, and caregivers play a pivotal role in navigating the complexities of this condition and ensuring the well-being of children affected by Kawasaki disease.