Congenital disorders
Spotlight on CLOVES syndrome
You’ve probably never heard of CLOVES syndrome. It’s a very rare genetic overgrowth disorder — so rare that fewer than 200 cases have been identified worldwide to date.
Researchers believe that mutations in the PIK3CA gene are at the root of the condition, which manifests in the form of fatty overgrowths and vascular and joint abnormalities. (The name of the syndrome — CLOVES — is an acronym that stands for congenital lipomatous overgrowth with vascular malformations, epidermal nevi, and scoliosis/skeletal/spinal anomalies.)
People with CLOVES have large masses of fatty tissue, complex vascular malformations, patches of overgrown skin, spine problems, other bone and joint abnormalities, and stiff or weak muscles. These symptoms can be present at birth or appear later in early childhood.
Interestingly, these overgrowth abnormalities may stop in childhood or continue into adulthood.
Today is CLOVES Syndrome Awareness Day. In observance, this article will cover the history of the condition, its genetic and molecular bases, and current treatment options.
Now and then
The condition was first described as a distinct syndrome in 2007 by Julie C. Sapp and a group of researchers from the National Human Genome Research Institute of the National Institutes of Health. They first coined the name congenital lipomatous overgrowth, vascular malformations, and epidermal nevi, or CLOVE.
The acronym was expanded in 2009 to CLOVES by Ahmad I. Alomari of Children’s Hospital Boston to emphasize the association of skeletal and spinal anomalies with the disease.
However, a case report by the German physician Hermann Friedberg titled “Gigantism of the right lower limb” published in 1867 is probably the first-known written account of the syndrome.
Part of a spectrum of diseases
CLOVES is part of the PIK3CA-related overgrowth spectrum, or PROS, which encompasses a range of genetic disorders that lead to the overgrowth and disfiguration of various body parts due to mutations in the gene PIK3CA.
These disorders have overlapping symptoms and common PIK3CA gene mutations in cells in the areas of the body that are affected.
Further, as spectrum disorders, all these are manifested in a broad range of symptoms and severity, and not all patients will have the same phenotype.
This is because genetic mutations that cause PROS are somatic mosaic mutations that occur sporadically and spontaneously in some cells during postzygotic embryo development in the womb. Therefore, mutations are not present in all cells, and only certain areas of the body are overgrown, ranging from isolated digits to whole limbs, the trunk, or the brain.
This large heterogeneity in symptoms makes it particularly difficult to create standard diagnoses, follow-ups, and classifications for these diseases.
As a disease caused by somatic PIK3CA mutations, the CLOVES is not inheritable. Moreover, as of now, there are no known risk factors that would make these mutations more or less likely to occur. Also, the disease affects males and females in equal probability.
Molecular basis
CLOVES syndrome is thought to arise from somatic activating mutations in the PIK3CA gene on chromosome 3 (3q26.32.6) during early embryonic development.
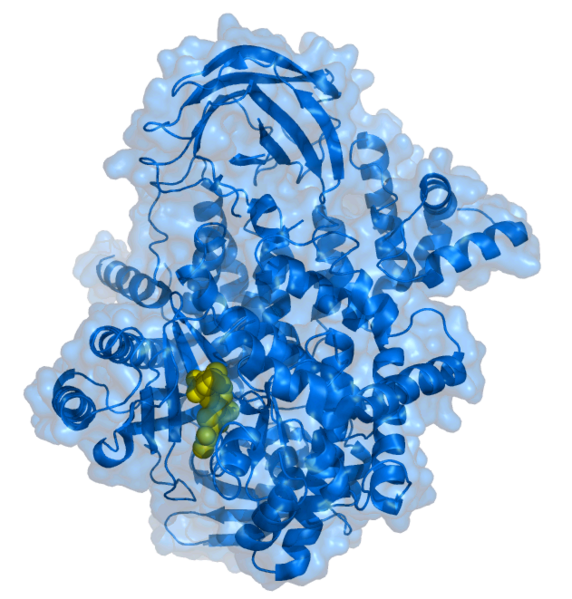
The human PIK3CA gene encodes the protein phosphatidylinositol-4,5-bisphosphate-3-kinase, or PIK3 subunit alpha, or PIK3CA/p110α. This is an upstream regulator of the PI3K/AKT/mTOR cell-signaling pathway.
This signaling pathway plays a critical role in cell-cycle control. It promotes cell growth and regulates its maturation, angiogenesis, survival and metabolism. The pathway consists of series of kinases that are regulated by phosphorylation and dephosphorylation by specific kinases, phosphatases, GTP/GDP exchange proteins, adaptor proteins and scaffolding proteins.
In general, signal transduction in PI3K/AKT/mTOR cell-signaling pathway initiates with the activation of transmembrane receptors such as receptor protein tyrosine kinases, or RTKs, and G-protein–coupled receptors, or GPCRs. Activation of RTK leads to an activation of PI3K with the PIK3CA catalytic domain by directly attaching one of the two SH2 domains in the adaptor subunit of PI3K (e.g. p85) to phosphotyrosine consensus residues of activated RTK. Activated PIK3CA then produces the second messenger phosphatidylinositol-3,4,5-triphosphate or PtdIns(3,4,5)P3 from the PtdIns(4,5)P2.
PtdIns(3,4,5)P3 then recruits a subset of signaling proteins with pleckstrin homology domains to the membrane, including protein serine/threonine kinase-3′-phosphoinositide-dependent kinase 1, or PDK1, and V-Akt murine thymoma viral oncogene homolog, or AKT.
This allows PDK1 to access and phosphorylate T308 in the activation loop of AKT. Activated AKT phosphorylates and inhibits tuberous sclerosis complex 2 and proline-rich Akt substrate of 40 kDa, leading to activation of the rapamycin complex 1, or mTORC1.
The mTORC1 substrates include the eukaryotic translation initiation factor 4E binding protein 1 and ribosomal protein S6-kinase-70 kDa-polypeptide-1, or S6K1, which in turn phosphorylates the ribosomal protein S6, or S6/RPS6, promoting protein synthesis and cellular proliferation.
Thus, activating mutations of PIK3CA overstimulate affected cells, leading to competitive growth and proliferation and metastatic capacity. De novo mutations in PIK3CA create an oncogenic gene with the capacity to promote many different types of cancer. However, when these mutations occur during embryogenesis, they lead to tumoral growth or overgrowth in solid organs, bone, muscle, lymphatic tissue and blood vessels as a result of two or more genetically distinct cell lineages.

A schematic of the PI3K/AKT/mTOR cell-signaling pathway.
Treatment options
Unfortunately, as of now, there is no cure for CLOVES syndrome. Surgical and other types of medical interventions are used to manage tissue overgrowth, vascular anomalies and other related medical issues. This requires a patient to have access to an interdisciplinary team of physicians with experience in overgrowth and vascular anomalies.
Debulking operations are performed to reduce the size of the tissue overgrowths. Orthopedic procedures are used to manage large limb anomalies. Large veins and lymphatic malformations are treated with minimally invasive procedures such as sclerotherapy, embolization and laser treatment before undergoing surgical procedures due to the risk of vein thrombosis.
However, as these abnormal tissues can often regrow, patients are required to undergo repeated surgical interventions during a lifetime.
To treat CLOVES and other diseases in the spectrum, research into pharmacological treatments capable of blocking the PIK/AKT/mTOR pathway has increased over the past decade with promising results.
Sirolimus (also known as rapamycin), an mTOR inhibitor, emerged as a treatment option for patients suffering from PROS in 2011. The drug has been shown to curb progression, improve lymphatic manifestations, and control symptoms.
ATP-competitive p110α inhibitor alpelisib was approved in 2022 by the U.S. Food and Drug Administration as a treatment for severe cases of PROS in adults and children two years of age or older.
Hopefully, with increased awareness and attention, more treatment options will become available to improve the quality of life of people suffering from this debilitating disease.