Blood, Health Care, Symptoms
What Is Normal Blood Sugar?
Blood glucose, commonly known as blood sugar, constitutes the predominant form of sugar present in your bloodstream. This vital energy source derives from the carbohydrates present in the foods you consume. The pivotal role of glucose lies in providing primary energy to the cells, tissues, and organs throughout your body.
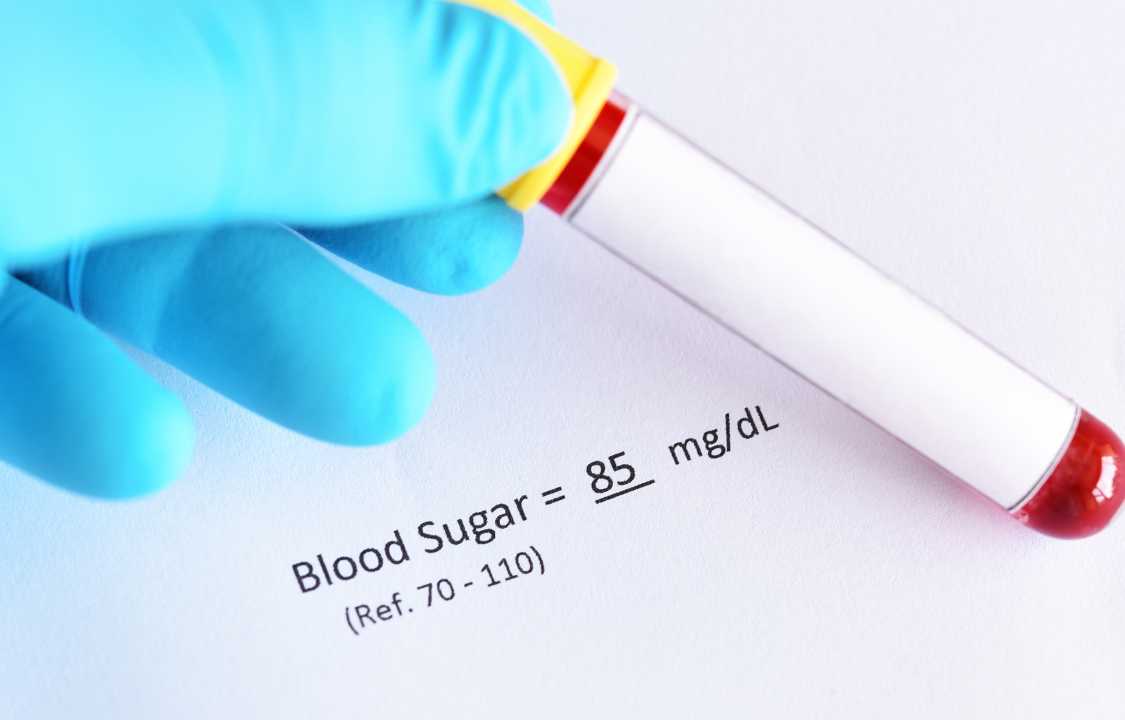
Maintaining a blood sugar level within the range of 70-99 mg/dL is considered normal. This range is subject to minor fluctuations over the course of a day in response to dietary intake. Nevertheless, the aim is to sustain blood sugar levels within this established range, minimizing the influence of dietary choices and physical activity on these fluctuations.
Vigilantly tracking your blood sugar levels holds the potential to avert severe complications, notably encompassing heart ailments and kidney disorders. This practice gains paramount importance for individuals managing diabetes, a chronic ailment characterized by an excess accumulation of glucose in the bloodstream.
Normal Blood Sugar Levels
Several variables have the potential to impact your blood sugar levels, encompassing alcohol consumption, specific antibiotics, and the concentration of insulin circulating in your blood. Insulin, a pivotal hormone, plays a vital role in the regulation of blood glucose levels.
Typical blood sugar thresholds are influenced by a variety of factors, such as:
- Age
- Degree of physical activity
- Stress levels
- Health conditions
- Medication usage
Outlined below are generalized benchmarks for blood sugar levels, expressed in milligrams per deciliter (mg/dL).
How Is Blood Sugar Tested?
A healthcare professional may suggest one or multiple tests to assess your blood sugar levels, aiding in the identification of prediabetes or diabetes. Prediabetes denotes a condition where blood sugar levels surpass normal but don’t yet reach the threshold for a diabetes diagnosis.
The categories of diabetes encompass:
1. Type 1: This autoimmune disorder involves the immune system erroneously targeting and impairing insulin-producing cells, resulting in insulin production cessation. Prevention of type 1 diabetes is not feasible.
2. Type 2: A persistent ailment marked by insufficient insulin production or improper utilization, leading to elevated blood sugar levels. Lifestyle modifications, including adopting a nutritious diet and engaging in regular physical activity, can prevent the onset of type 2 diabetes.
3. Gestational: Occurring during pregnancy, this form of diabetes involves elevated blood sugar levels which typically resolve after childbirth.
An endocrinologist, a medical professional specializing in hormonal matters, plays a pivotal role. Upon diabetes or prediabetes diagnosis, collaborating with an endocrinologist is customary. Regular blood sugar monitoring is also likely to be initiated, ensuring continuous tracking throughout the day.
In-Office Testing
Evaluating your blood sugar is a straightforward process, yielding prompt results. Various tests administered in a healthcare setting include the A1C test, fasting plasma glucose (FPG) test, and the oral glucose tolerance test (OGTT).
A1C: Also recognized as the hemoglobin A1C or HbA1c test, a small blood sample is taken from your arm or finger by your healthcare provider. This assessment determines your average blood sugar levels over the preceding three months. The procedure can be conducted within the office or a laboratory and necessitates no prior preparation.
FPG: This examination gauges your blood glucose concentrations after a fasting period of at least eight hours. You’re required to abstain from eating or drinking anything, except water, for this duration preceding the test. Typically, the test is performed upon waking in the morning.
OGTT: Employed frequently for gestational diabetes screening, this test involves adhering to a regular carbohydrate diet for three days before the examination, followed by fasting for 10-16 hours. During the appointment, a baseline blood sample is drawn using a needle. Subsequently, you’ll consume a glucose solution. Depending on the specific protocol, additional blood samples might be collected at intervals of 30, 60, 90, or 120 minutes to observe your body’s response to the glucose load. Diverse versions of the test exist, encompassing variations in glucose dosages and sampling timeframes.
At-Home Testing
You have the option of employing a compact and portable tool known as a blood sugar meter (also called a glucometer) to self-monitor your blood sugar levels at home. These meters come in various types and can be purchased from various outlets, including online platforms and nearby pharmacies. They typically function similarly and come equipped with a lancing device referred to as a lancet. Remember to procure additional lancets and test strips to ensure an ongoing supply.
Follow these steps to effectively monitor your blood sugar using your glucometer:
1. Ensure the cleanliness of the machine.
2. Take out a single test strip from its packaging and seal the package immediately to avoid moisture damage.
3. Thoroughly wash your hands with soap and dry them. Gently massage the selected finger to enhance blood circulation in that area.
4. Employ a lancet to prick your finger.
5. Apply a small drop of blood onto the test strip or touch the strip’s edge to the blood drop.
6. Insert the test strip into the meter and await the results, which will become visible within a few seconds.
7. Safely discard the used lancet and test strip.
You can maintain a record of your outcomes using a smartphone application or a physical record that you can bring to your healthcare appointments. This record is likely to encompass your blood glucose levels both before meals and 1-2 hours after eating.
To ensure safety and efficacy:
- Do not share lancets with others.
- Make certain that someone familiar with your glucometer’s operation, such as a household member, can use it to monitor your blood sugar in case you fall ill.
Who Might Need a Blood Sugar Test?
A blood sugar test could be administered by your healthcare professional under the following circumstances:
1. Symptoms Indicative of Blood Sugar Imbalance: If you exhibit signs of elevated or decreased blood sugar levels.
2. Elevated Risk of Diabetes: In case you possess an escalated susceptibility to developing diabetes due to certain risk factors.
3. Pregnancy: If you are pregnant, monitoring blood sugar levels is particularly relevant.
Following the test, a dialogue will take place to determine the subsequent actions tailored to your situation. These potential actions could encompass further diagnostic assessments, prescribed medications, and modifications to your lifestyle. You might also receive recommendations to regularly monitor your blood glucose levels, which is particularly pertinent if:
- You rely on insulin treatment.
- You encounter challenges in achieving your target glucose range.
- You experience low blood sugar levels, with or without conventional symptoms.
- You are in a pregnant state.
Abnormal Blood Sugar
Elevated blood sugar, known as hyperglycemia, manifests as a fasting blood glucose level ranging from 100 to 125 mg/dL, which signifies a state of prediabetes. Crossing the threshold of 125 mg/dL indicates diabetes, amplifying the vulnerability to conditions such as heart disease and stroke.
Conversely, reduced blood sugar, termed hypoglycemia, emerges with a fasting blood sugar measurement below 70 mg/dL. If blood glucose levels plummet significantly, dipping below 54 mg/dL, the potential for complications escalates, potentially leading to adverse events like fainting and seizures.
High Blood Sugar
Elevated blood sugar, known as hyperglycemia, manifests as a fasting blood glucose level Hyperglycemia can manifest irrespective of diabetes and is sometimes provoked by factors such as stress or illness, according to information from MedlinePlus.
For individuals managing diabetes, various factors can trigger spikes in blood sugar levels. Examples encompass inadequate insulin administration, inefficacious insulin utilization (insulin resistance), and insufficient physical activity to support overall well-being. Additional potential catalysts include sunburns, artificial sweeteners, coffee consumption, inadequate sleep, skipping breakfast, dehydration, nasal spray usage, and gum disease.
Recognizable indications of elevated blood sugar encompass:
1. Vision disturbances
2. Excessive thirst or dry mouth
3. Dry skin
4. Sensations of weakness or fatigue
5. Frequent urination (polyuria)
Hyperglycemia management is contingent on the specific blood sugar level. Engaging in exercise, for instance, can lower blood glucose levels for up to 24 hours, influenced by individual insulin sensitivity.
However, if blood sugar surpasses 240 mg/dL, the presence of ketones may be detected in urine. Ketones emerge when the body breaks down fat for energy due to insufficient glucose availability. Engaging in exercise can promote ketone production as it demands energy. Elevated ketone levels might lead to a critical medical state known as diabetic ketoacidosis (DKA).
To avert complications associated with heightened blood sugar, it is recommended to consult your healthcare provider. They might make adjustments to your medication or insulin regimen or refer you to a registered dietitian (RD). An RD possesses specialized expertise in diet and nutrition and can assist in crafting a meal plan to maintain stable blood glucose levels.
Low Blood Sugar
Hyperglycemia can manifest irrespective of diabetes and is sometimes provoked by factors such as stress or illness, according to information from MedlinePlus.
For individuals managing diabetes, various factors can trigger spikes in blood sugar levels. Examples encompass inadequate insulin administration, inefficacious insulin utilization (insulin resistance), and insufficient physical activity to support overall well-being. Additional potential catalysts include sunburns, artificial sweeteners, coffee consumption, inadequate sleep, skipping breakfast, dehydration, nasal spray usage, and gum disease.
Recognizable indications of elevated blood sugar encompass:
1. Vision disturbances
2. Excessive thirst or dry mouth
3. Dry skin
4. Sensations of weakness or fatigue
5. Frequent urination (polyuria)
Hyperglycemia management is contingent on the specific blood sugar level. Engaging in exercise, for instance, can lower blood glucose levels for up to 24 hours, influenced by individual insulin sensitivity.
However, if blood sugar surpasses 240 mg/dL, the presence of ketones may be detected in urine. Ketones emerge when the body breaks down fat for energy due to insufficient glucose availability. Engaging in exercise can promote ketone production as it demands energy. Elevated ketone levels might lead to a critical medical state known as diabetic ketoacidosis (DKA).
To avert complications associated with heightened blood sugar, it is recommended to consult your healthcare provider. They might make adjustments to your medication or insulin regimen or refer you to a registered dietitian (RD). An RD possesses specialized expertise in diet and nutrition and can assist in crafting a meal plan to maintain stable blood glucose levels.
Hypoglycemia can manifest both in individuals with or without diabetes.
Factors contributing to low blood sugar encompass:
- Certain categories of diabetes medications and other pharmaceuticals
- Alcohol consumption
- Insulinoma (an infrequent pancreatic tumor)
- Insufficiency of hormones like cortisol, growth hormone, or thyroid hormone
- Conditions such as heart, kidney, or liver failure
- Prior history of weight-loss surgeries
While some individuals may not display explicit symptoms of low blood sugar, potential indicators can include:
- Impaired vision
- Accelerated heart rate
- Excessive sweating
- Headaches
- Fatigue
- Irritability
- Tingling or numbness
- Cognitive difficulties
Though low blood sugar can pose risks, it is manageable. The “15-15 rule” can be followed when glucose levels fall within the range of 55 to 69 mg/dL: Consume 15 grams of carbohydrates with low fiber and fat content, and repeat this intake every 15 minutes until your blood sugar exceeds 70 mg/dL. It’s crucial to opt for carbohydrates with minimal fiber and fat as these components slow down digestion, meaning foods like beans or chocolate are not suitable for rapidly restoring blood sugar levels.
Carbohydrate options include:
- 4 ounces (oz) of juice
- 1 tablespoon of sugar, honey, or maple syrup
- 6-7 hard candies
- 3 glucose tablets (chewable sugar tablets)
For young children, the required carbohydrate intake is typically lower, thus consulting their doctor for specific guidance is recommended.
In instances where blood sugar drops below 55 mg/dL, contacting emergency services (911) is advisable. Additionally, if you possess an injectable glucagon kit at home, it can be used as an emergency medication.
A Quick Review
Glucose, commonly known as blood sugar, serves as the primary form of sugar circulating in your bloodstream. It functions as the energy source for your body, deriving from the foods you consume.
Sustaining balanced blood sugar levels is crucial, particularly if you are managing diabetes. Should you encounter symptoms suggestive of elevated or diminished blood sugar, it is advisable to promptly seek guidance from a healthcare professional. Neglecting to address these symptoms could potentially expose you to an array of complications.
The process of testing your blood glucose level is both swift and uncomplicated. This assessment can be conducted in the comfort of your home or within a healthcare setting, with instant access to your results.