Infection
Pocket-Sized Device Uses Heat Signatures and Bacterial Fluorescence to Identify Infected Wounds Faster
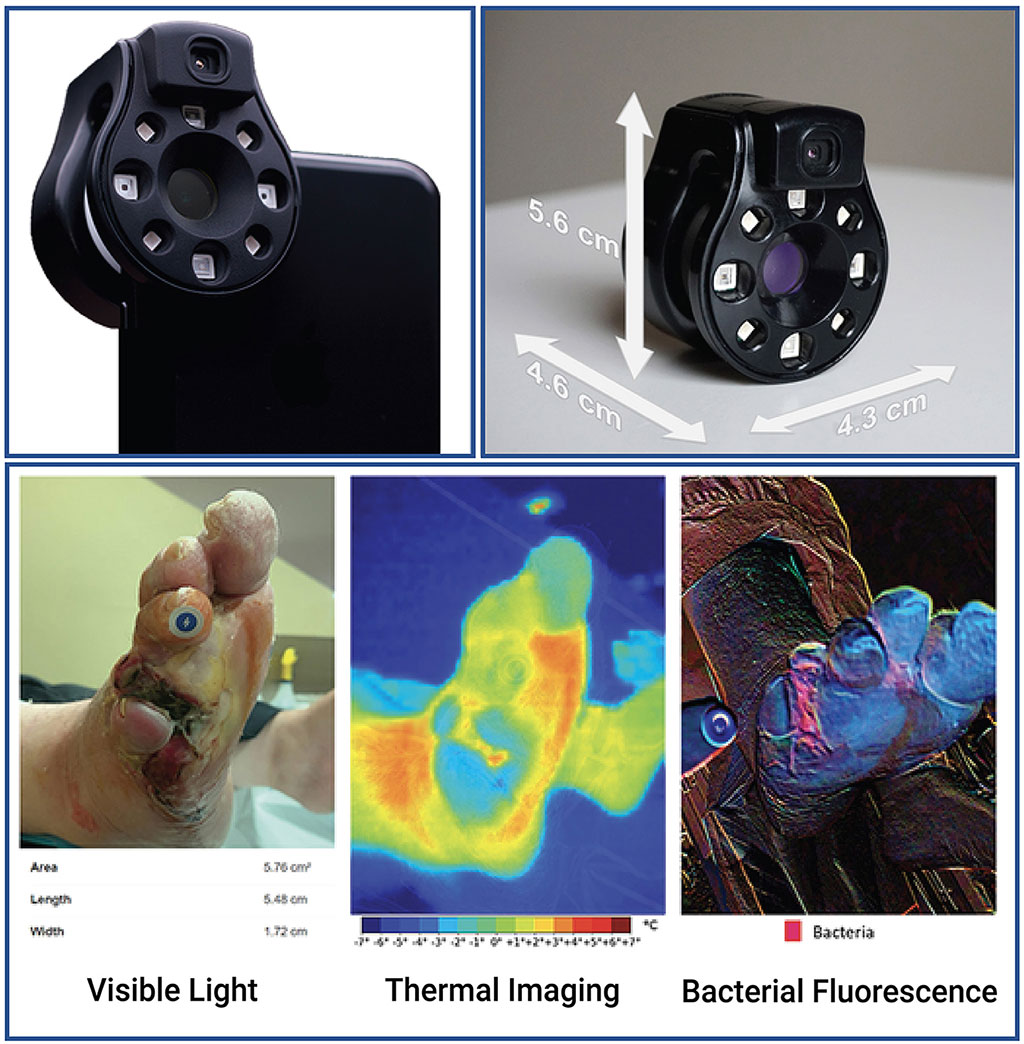
Image: The Ray 1 hyperspectral imaging device (Photo courtesy of Frontiers in Medicine)
Identifying a wound that is becoming infected has long posed challenges for medical professionals. The signs and symptoms are often vague, and methods of detecting bacteria are time-consuming and not always accessible. Consequently, diagnosing a wound infection can be subjective, depending upon the experience of clinicians. The risk of infections delaying the healing process or spreading within the body underscores the urgency of timely treatment to ensure the well-being of patients. Now, an international team of scientists and clinicians have developed a device run from a smartphone or tablet app that enables advanced imaging of a wound in order to identify infection.
Scientists at Western University (Toronto, ON, Canada) and Swift Medical (Toronto, ON, Canada) have built a device that works with smartphones and tablets to capture medical images capable of identifying infected wounds. By capturing both the heat emitted by a wound and the fluorescence of bacteria, this device aids clinicians in distinguishing between inflammation and a potentially dangerous infection. This advancement could expedite interventions, enabling the identification of infections before they escalate into severe health risks. Dubbed the Swift Ray 1, the device attaches to a smartphone and interfaces with the Swift Skin and Wound software. This pairing facilitates the capture of medical-grade photos, infrared thermography images (which measure body heat), and bacterial fluorescence images (which reveal bacteria using violet light).
None of these images, taken individually, would be sufficient to confirm infection. Clinical examination has limited accuracy, as does thermography, which detects heat variations due to inflammation and infection. Bacterial fluorescence alone can only evaluate the wound’s surface, which is naturally colonized by bacteria, creating the need for additional methods to differentiate between contamination and an infected wound. The researchers set out to combine these modalities in order to devise an approach that wouldn’t require multiple costly devices, would address the shortcomings of each imaging method, and could provide an objective measure of the wound healing progress. To validate their device, they recruited 66 patients with wounds meeting specific criteria. These wounds exhibited no signs of infection spreading, did not contain foreign objects, and had not previously been treated with antibiotics or growth factors. After uncovering, cleaning, and drying the wounds, imaging was performed, followed by routine care.
A researcher who was not present for the wound care process reviewed the images and identified four distinct patterns. Wounds with normal temperature and no bacterial fluorescence were deemed ‘non-inflamed’, while slightly warmer wounds with minimal bacterial fluorescence were categorized as ‘inflamed’. The last two patterns, characterized by significantly elevated temperature, with or without bacterial fluorescence, were both labeled as ‘infected’, based on the unanimous opinion of clinicians who examined these wounds. Among the 66 wounds, 20 were classified as non-inflamed, 26 as inflamed, and 20 as infected.
To evaluate the device’s accuracy, the researchers conducted a principal component analysis and employed the nearest k-neighbor clustering algorithm to assess whether a machine learning model could correctly differentiate these wound categories. Impressively, the model successfully distinguished all three categories with an overall accuracy of 74%. When distinguishing between infected and non-infected wounds, the model accurately identified 100% of infected wounds and 91% of non-infected wounds. The researchers underscored the importance of considering these images within a medical context. For instance, a wound deemed cool enough to be non-inflamed might have compromised blood supply affecting healing. However, the combination of the Swift Ray 1 device with the Swift Skin and Wound software enables doctors to merge multiple infection identification methods, expanding their diagnostic toolkit without the need for multiple expensive devices. In the future, this technology could enable swift, accurate diagnoses for every patient with wounds, and facilitate more effective telemedicine assessments.
“Research has demonstrated bacterial imaging helps guide clinicians’ work to remove nonviable tissue, yet it cannot identify infection by itself,” said Dr. Jose Ramirez-GarciaLuna of McGill University Health Centre, first author of the study. “Thermography provides insight into the inflammatory and circulatory changes happening under the skin.”
Related Links:
Western University
Swift Medical