Infection
Fewer adults hospitalized with COVID-19 had critical outcomes as pandemic progressed
September 22, 2023
2 min read
Source/Disclosures
Published by:
Disclosures:
Tenforde reports no relevant financial disclosures. Please see the study for all other authors’ relevant financial disclosures.
Key takeaways:
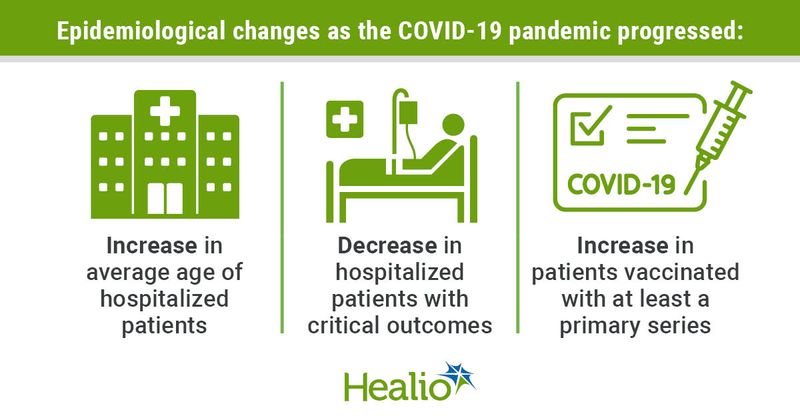
- The age of patients hospitalized with COVID-19 has increased throughout the pandemic.
- The overall proportion of ICU admissions, respiratory failure and deaths decreased.
Adults hospitalized with COVID-19 were less likely to experience critical outcomes such as ICU admission, respiratory failure or death during later periods of the pandemic, researchers found.
“There is a need to understand how the clinical epidemiology of COVID-19 has changed over time, particularly in response to emergence of new SARS-CoV-2 variants, increasing levels of population immunity through vaccination or prior infections, and advances in clinical care,” Mark Tenforde, MD, medical officer at the CDC’s National Center for Immunization and Respiratory Diseases, told Healio.
To help better understand these possible changes, Tenforde and colleagues assessed adults aged 18 years and older from 10 states who were hospitalized with COVID-19 between June 2021 and March 2023.
According to the study, the researchers evaluated changes in baseline demographic and clinical characteristics and critical outcomes — such as ICU admission and death — and used regression models to evaluate critical outcomes risk factors in relation to COVID-19 vaccination status.
In total, more than 60,000 COVID-19-associated hospitalizations were assessed and showed that the epidemiology of COVID-19 “changed markedly” over time.
Among patients hospitalized, the median age of patients increased from 60 to 75 years, the proportion of patients vaccinated increased from 18.2% to 70.1% and reports of critical outcomes declined from 24.8% to 19.4%. Of more than 13,000 critical outcomes reported, there were 18.9 were admitted to the ICU and 9.4% died, whereas 14.2% required the use of noninvasive mechanical ventilation and 10.7% required invasive mechanical ventilation, all of which the researchers said decreased in later periods of the pandemic.
The study also showed that demographic characteristics of hospitalized patients followed similar patterns as COVID-19 hospitalizations in general.
According to the study, patients with critical illness had a higher proportion of people with four or more underlying medical condition categories compared with those without critical illness (32.8% vs. 23%), as well as immunocompromising conditions (17.9% vs. 13.3%), whereas a smaller proportion were vaccinated with at least a primary series (34.9% vs. 41.9%).
“The clinical takeaway is to remain vigilant in protecting and caring for groups such as older adults and those with multiple health issues,” Tenforde said. “Crucial tools are available to reduce the risk of severe COVID-19 outcomes including increasing COVID-19 vaccine uptake and using effective antiviral therapies.”