Brain, Disease, Inflammation
Fungal Meningitis: What to Know About the Recent Outbreak Linked to Mexican Clinics
In recent times, a grave health concern has gripped the attention of the Centers for Disease Control and Prevention (CDC) – a fungal meningitis outbreak linked to two clinics in Matamoros, Mexico. This alarming situation has the potential to affect nearly 200 Americans, shedding light on the perils of fungal meningitis and the importance of healthcare provider awareness and a vigilant environment.
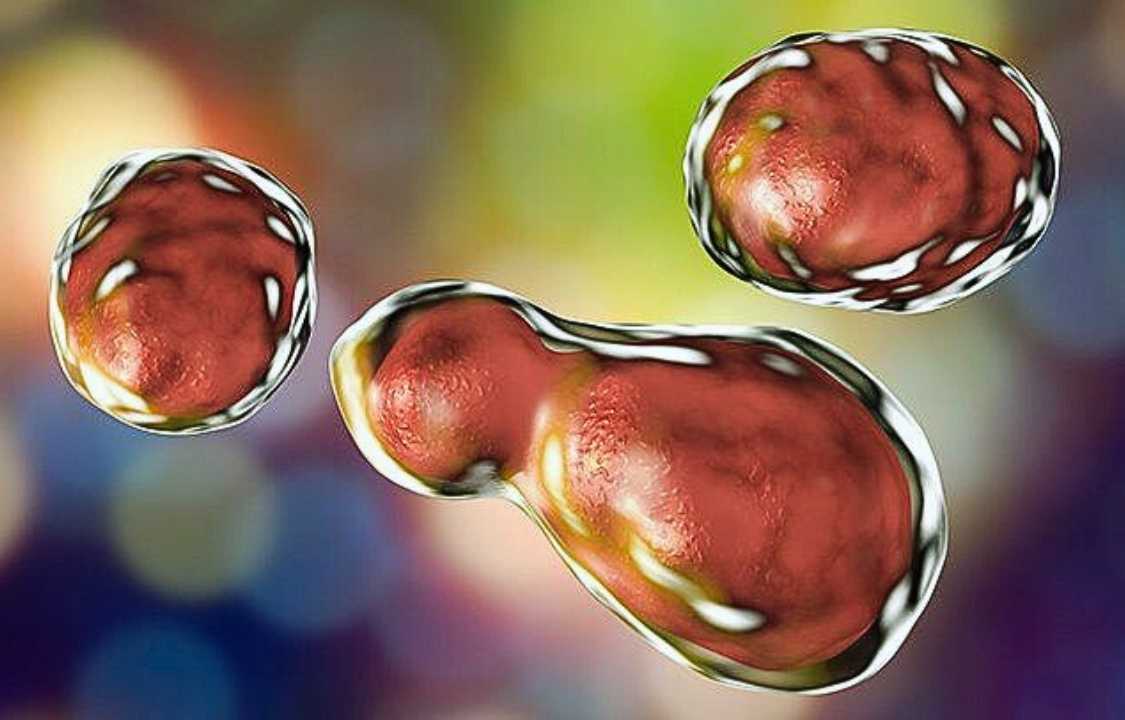
Understanding Fungal Meningitis: A Lethal Threat
Fungal meningitis is a formidable adversary – a potentially fatal infection and inflammation that targets the brain and spinal cord. However, it does not possess the sinister attribute of person-to-person transmission. Instead, this treacherous ailment is contracted through the inhalation of fungal spores present in one’s environment.
The CDC’s estimations reveal that this outbreak has cast its ominous shadow over nearly 200 Americans. These individuals may have been exposed to the fungal menace after receiving epidural anesthesia in preparation for cosmetic procedures at two clinics situated in Matamoros, Tamaulipas, Mexico – a city adjacent to Brownsville, Texas.
The CDC, in its advisory role, implores anyone who sought medical care at either River Side Surgical Center or Clinica K-3, both in Matamoros, during the timeframe of January 1 to May 13, 2023, to undergo an evaluation for meningitis at the nearest emergency room. This recommendation holds true even for those who are currently asymptomatic. Additionally, individuals should disclose their visit to one of these clinics and their associated risk to their healthcare providers.
Dr. Peter Pappas, an infectious disease specialist at UAB Medicine in Alabama, underscores the critical nature of this advisory. He emphasizes that this proactive approach serves as a crucial means of identifying and intercepting potential cases in their early stages, preventing the infection from significantly impacting the brain.
Early Signs and Symptoms of Fungal Meningitis
Early symptoms of fungal meningitis connected to this outbreak encompass redness and pain at the injection site. If detected promptly, these symptoms can be effectively treated before the infection infiltrates the brain. However, the concern deepens when more invasive symptoms manifest weeks after exposure. These symptoms include headaches, a stiff neck, and a low-grade fever on the milder side. On the extreme end of the spectrum, fungal meningitis can lead to stroke and altered brain function. The mortality rate for this specific outbreak stands at a harrowing 40%, as elucidated by Dr. Pappas.
While the gravity of these infections cannot be understated, it is essential to note that fungal meningitis is not contagious. Individuals who have not visited the implicated clinics during the specified timeframe are not at risk and need not take preventive measures against infection.
Fungal Meningitis Treatment: A Complex Challenge
Various pathogens, including bacteria, viruses, parasites, and fungi, can precipitate meningitis, all of which are a cause for concern due to their potential long-lasting effects on brain function, according to Dr. Stuart Levitz, a professor of medicine at UMass Chan Medical School.
Fungal meningitis, in particular, poses a significant treatment challenge. Dr. Levitz explains that there are fewer antifungal drugs available compared to antibacterial drugs, and some antifungal medications struggle to penetrate the brain effectively. Furthermore, fungal meningitis symptoms typically take weeks to develop, in stark contrast to bacterial meningitis, which often manifests within a week of exposure.
The organism responsible for this outbreak, Fusarium solani, is notoriously resilient and difficult to treat. This same fungus was the culprit behind a previous outbreak traced to a hospital in Durango, Mexico, in December, claiming the lives of 35 patients, primarily pregnant women who had received epidurals.
Dr. Pappas emphasizes the challenges in treating this formidable pathogen, noting that treatment options are limited, and the infection becomes more entrenched and invasive over time, making it increasingly challenging to combat.
The Genesis of Fungal Meningitis: Unmasking the Culprit
Typically, fungal meningitis arises when a fungal infection spreads through the bloodstream and infiltrates the brain, where it initiates meningitis. These infections predominantly afflict individuals with compromised immune systems, such as those with HIV/AIDS or recipients of organ transplants on immunosuppressive medications.
However, the recent outbreak paints a different picture. In the two clinics associated with this outbreak, individuals received anesthesia via epidurals. While the precise cause remains under investigation, Dr. Levitz suggests that either the needle or the anesthesia drugs may not have been sterile, potentially harboring fungal contamination that was directly injected into the cerebrospinal fluid, offering a direct route to the brain.
Such outbreaks arising from contaminated medical equipment are not isolated incidents, as exemplified by a 2012 outbreak linked to steroid injections for pain administered at the New England Compounding Center in Framingham, Massachusetts. Dr. Levitz emphasizes that this issue is not unique to medical tourism in Mexico but is more likely the result of cost-saving measures involving medications meant for single use being reused. In some cases, equipment may be contaminated before reaching the medical facility, unbeknownst to the healthcare professionals.
Despite the alarming nature of this outbreak, Dr. Levitz offers a glimmer of hope, highlighting that the source has been identified, and the number of new cases is expected to decline significantly.
The Imperative of Awareness: Knowing Your Healthcare Provider and Environment
The recent outbreak serves as a poignant reminder of the vital importance of awareness regarding one’s healthcare provider and the environment in which medical procedures are conducted. Dr. Pappas underscores the need to know and trust one’s physician, healthcare provider, and clinic, particularly when undergoing procedures involving epidurals.
In conclusion, the fungal meningitis outbreak originating from two clinics in Matamoros, Mexico, is a sobering reminder of the critical role awareness plays in healthcare. This ominous event highlights the need for stringent adherence to sterile techniques and vigilant oversight of medical equipment, underscoring the shared responsibility of healthcare providers and patients in safeguarding health and well-being.