Ovarian cancer, a formidable adversary in the realm of oncology, arises from the uncontrolled growth of abnormal cells within or around the ovaries, culminating in the formation of a tumor. Its prevalence is a stark reality, affecting approximately 1.1% of individuals with ovaries during their lifetime. This insidious disease presents a unique challenge in the medical field due to the absence of a reliable screening test for asymptomatic individuals, making early detection a significant challenge. When ovarian cancer is suspected, healthcare providers embark on a diagnostic journey, beginning with a thorough medical history assessment.
Medical History: The foundation of the diagnostic process lies in understanding an individual’s personal and family medical history. This step is crucial in assessing risk factors associated with ovarian cancer, especially when there is a family history of breast or ovarian cancer, as these malignancies can have a hereditary component. Additionally, if an individual presents with symptoms indicative of ovarian cancer, the healthcare provider delves into when these symptoms commenced and their frequency.
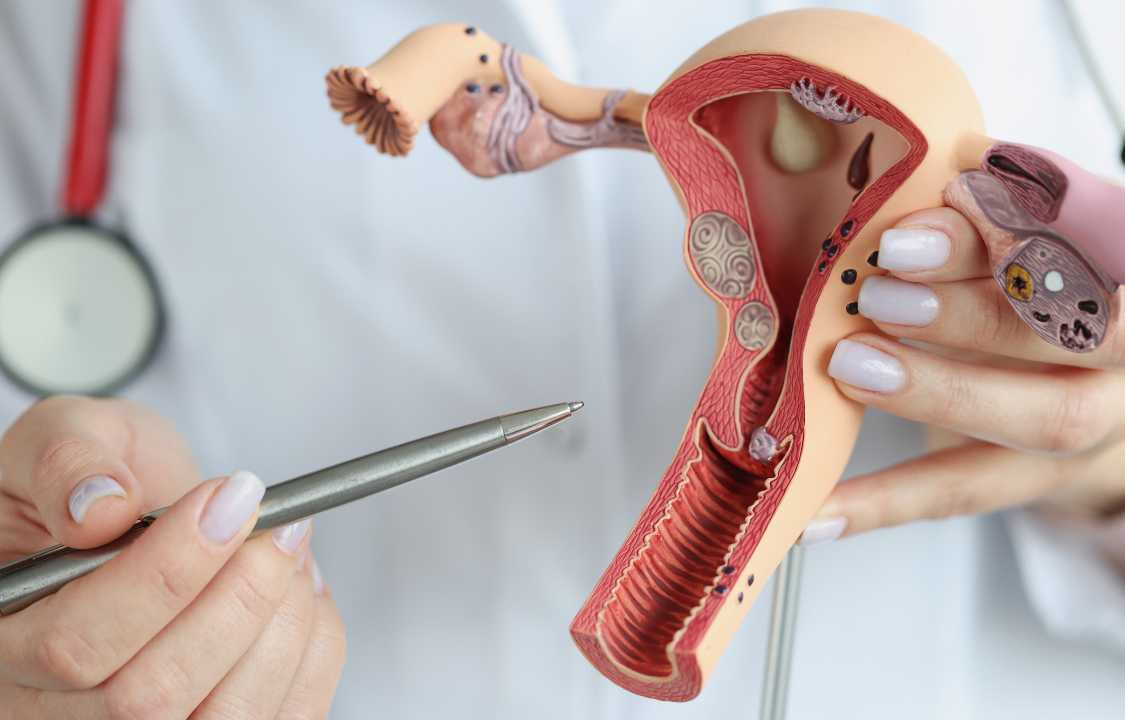
Pelvic Exam: A pivotal component of the diagnostic protocol is the pelvic exam, which involves a physical examination of the pelvic region. During this examination, the healthcare provider assesses for signs of ovarian cancer, such as the presence of fluid within the abdomen and the presence of lumps around the ovaries. This tactile examination allows them to gauge the size, shape, and position of the ovaries and uterus. However, it’s important to note that detecting ovarian cancer through pelvic exams in the early stages is rare, as most tumors are too small to be palpable.
Imaging: The realm of medical imaging plays a crucial role in the diagnosis of ovarian cancer. These imaging modalities utilize various forms of energy, such as sound waves and X-rays, to capture images of the internal structures within the body. They enable healthcare providers to visualize masses (tumors) within the ovaries, fallopian tubes, or the peritoneum lining the abdominal organs and cavity.
Transvaginal Ultrasound: Employing sound waves, a transvaginal ultrasound provides detailed images of the pelvic organs and structures. By inserting a probe into the vagina, healthcare providers gain a clear view of the ovaries and uterus, aiding in the detection of masses in this region. Additionally, it allows for an estimation of the mass’s size and differentiation between solid tumors and fluid-filled cysts. This imaging method also helps identify pelvic fluid accumulation, often observed in advanced ovarian cancers.
Computed Tomography (CT) Scan: CT scans utilize X-rays to produce cross-sectional images of the abdomen and pelvis. While they serve a diagnostic role in ovarian cancer, their primary utility lies in evaluating the extent of cancer spread, known as metastasis, to areas like lymph nodes, the liver, intestines, and other organs. In some cases, CT scans also guide needle biopsies, aiding in tissue sample collection for subsequent laboratory analysis to confirm malignancy.
Magnetic Resonance Imaging (MRI) Scan: MRI scans create cross-sectional images of the body, offering high accuracy in distinguishing between malignant and benign masses. While not typically the initial imaging choice for ovarian cancer detection, MRIs excel in providing additional information about masses identified through other imaging techniques. Furthermore, MRIs are valuable in assessing cancer spread to distant areas, such as the spinal cord and brain.
Blood Tests: In addition to physical exams and imaging, blood tests are essential components of the diagnostic process. They provide insights into overall health, kidney and liver function, and blood cell counts, including red blood cells, white blood cells, and platelets. The CA-125 blood test is particularly pertinent to ovarian cancer diagnosis.
CA-125 Blood Test: This test measures the concentration of cancer antigen 125 (CA-125), a protein elevated in a significant percentage of individuals with ovarian cancer. It is not a standalone diagnostic tool but serves as a valuable marker to monitor treatment effectiveness and disease recurrence. Elevated CA-125 levels can also result from conditions other than ovarian cancer, such as endometriosis, pelvic inflammatory disease, and uterine fibroids.
Other Tumor Marker Blood Tests: When imaging reveals a mass in the ovarian region, healthcare providers may order additional blood tests to identify specific tumor markers indicative of the type of ovarian cancer. These markers can include alpha-fetoprotein (AFP), human chorionic gonadotropin (hCG), inhibin, and lactate dehydrogenase (LDH), each providing valuable insights into the cancer’s nature.
Surgical Biopsy: Definitive diagnosis of malignancy or benignity can only be achieved through a biopsy. In ovarian cancer cases, biopsies are often performed during surgical interventions. Tissue samples extracted from the tumor are meticulously examined by pathologists, specialists in scrutinizing body tissues and fluids, to confirm the presence of cancer cells.
Paracentesis: Some individuals with ovarian cancer develop ascites, an abnormal accumulation of fluid within the abdomen. When surgery is not a feasible option, healthcare providers may conduct a paracentesis. This procedure involves inserting a needle into the abdominal wall to retrieve a sample of the abdominal fluid. Laboratory analysis of this fluid can determine the presence of cancer cells.
Laparoscopy: In cases where surgery is not immediately indicated, laparoscopy may be employed to obtain tissue samples. This minimally invasive procedure entails making a small abdominal incision and introducing a slender tube equipped with a camera (laparoscope). The camera facilitates visual inspection of the abdomen and pelvis for suspected cancerous masses. If necessary, a second incision may be made to obtain tissue samples from tumors or lymph nodes for subsequent laboratory analysis.
Colonoscopy: While primarily employed in the diagnosis of colorectal cancer, a colonoscopy may also be utilized in suspected cases of ovarian cancer to ascertain the extent of cancer spread. The procedure involves the insertion of a colonoscope, equipped with a camera, through the anus, rectum, and large intestine. It allows for the visualization of lumps and masses, and tissue samples can be extracted for examination.
Genetic Testing: Genetic testing assumes significance in cases of ovarian cancer, especially when there is a suspicion of hereditary factors. Up to 25% of ovarian cancers are believed to have a hereditary component. These tests typically involve collecting blood, saliva, or cheek cell samples. Notably, the BRCA1 and BRCA2 mutations are well-known genetic changes associated with ovarian cancer. Understanding genetic mutations can guide treatment decisions and provide insights into an individual’s susceptibility to other cancer types.
Stages of Ovarian Cancer: Following a confirmed diagnosis, oncologists delve into determining the stage of ovarian cancer. Staging is a pivotal aspect of the diagnostic process, as it categorizes the cancer’s size and extent of spread. There are four stages of ovarian cancer, ranging from localized disease (Stage 1) to advanced metastatic cancer (Stage 4). Staging plays a pivotal role in devising treatment plans and predicting prognosis.
Screening for Related Conditions: The symptoms of ovarian cancer, such as abdominal pain, bloating, and frequent urination, often overlap with those of other medical conditions. Healthcare providers employ a battery of tests, including imaging, blood work, and procedures, to rule out other potential causes of these symptoms. Conditions that can mimic ovarian cancer symptoms include colon cancer, ectopic pregnancy, endometriosis, irritable bowel syndrome (IBS), ovarian cysts, urinary tract infections, and uterine fibroids.
Managing Breast Cancer Risk: Individuals diagnosed with ovarian cancer, particularly those with hereditary forms associated with BRCA1 or BRCA2 mutations, face an increased risk of developing breast cancer. To address this risk, healthcare providers may recommend a range of strategies, including more frequent breast cancer screenings (mammograms), prophylactic medications, or risk-reducing surgeries.
In summary, the diagnosis of ovarian cancer is a multifaceted process that relies on a combination of medical history assessment, physical examinations, medical imaging, blood tests, and tissue biopsies. The intricate interplay of these diagnostic tools is essential for accurate identification of the disease, determination of its stage, and formulation of a tailored treatment plan. Ovarian cancer is a complex adversary, but with early detection and precise diagnosis, individuals and their healthcare teams can embark on a journey toward effective management and improved outcomes.