Infection
Unrealized targets in the discovery of antibiotics for Gram-negative bacterial infections
Abstract
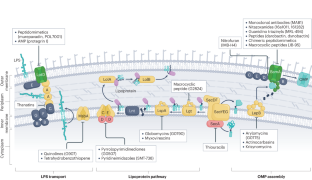
Advances in areas that include genomics, systems biology, protein structure determination and artificial intelligence provide new opportunities for target-based antibacterial drug discovery. The selection of a ‘good’ new target for direct-acting antibacterial compounds is the first decision, for which multiple criteria must be explored, integrated and re-evaluated as drug discovery programmes progress. Criteria include essentiality of the target for bacterial survival, its conservation across different strains of the same species, bacterial species and growth conditions (which determines the spectrum of activity of a potential antibiotic) and the level of homology with human genes (which influences the potential for selective inhibition). Additionally, a bacterial target should have the potential to bind to drug-like molecules, and its subcellular location will govern the need for inhibitors to penetrate one or two bacterial membranes, which is a key challenge in targeting Gram-negative bacteria. The risk of the emergence of target-based drug resistance for drugs with single targets also requires consideration. This Review describes promising but as-yet-unrealized targets for antibacterial drugs against Gram-negative bacteria and examples of cognate inhibitors, and highlights lessons learned from past drug discovery programmes.
This is a preview of subscription content, access via your institution
Access options
style{display:none!important}.LiveAreaSection-193358632 *{align-content:stretch;align-items:stretch;align-self:auto;animation-delay:0s;animation-direction:normal;animation-duration:0s;animation-fill-mode:none;animation-iteration-count:1;animation-name:none;animation-play-state:running;animation-timing-function:ease;azimuth:center;backface-visibility:visible;background-attachment:scroll;background-blend-mode:normal;background-clip:borderBox;background-color:transparent;background-image:none;background-origin:paddingBox;background-position:0 0;background-repeat:repeat;background-size:auto auto;block-size:auto;border-block-end-color:currentcolor;border-block-end-style:none;border-block-end-width:medium;border-block-start-color:currentcolor;border-block-start-style:none;border-block-start-width:medium;border-bottom-color:currentcolor;border-bottom-left-radius:0;border-bottom-right-radius:0;border-bottom-style:none;border-bottom-width:medium;border-collapse:separate;border-image-outset:0s;border-image-repeat:stretch;border-image-slice:100%;border-image-source:none;border-image-width:1;border-inline-end-color:currentcolor;border-inline-end-style:none;border-inline-end-width:medium;border-inline-start-color:currentcolor;border-inline-start-style:none;border-inline-start-width:medium;border-left-color:currentcolor;border-left-style:none;border-left-width:medium;border-right-color:currentcolor;border-right-style:none;border-right-width:medium;border-spacing:0;border-top-color:currentcolor;border-top-left-radius:0;border-top-right-radius:0;border-top-style:none;border-top-width:medium;bottom:auto;box-decoration-break:slice;box-shadow:none;box-sizing:border-box;break-after:auto;break-before:auto;break-inside:auto;caption-side:top;caret-color:auto;clear:none;clip:auto;clip-path:none;color:initial;column-count:auto;column-fill:balance;column-gap:normal;column-rule-color:currentcolor;column-rule-style:none;column-rule-width:medium;column-span:none;column-width:auto;content:normal;counter-increment:none;counter-reset:none;cursor:auto;display:inline;empty-cells:show;filter:none;flex-basis:auto;flex-direction:row;flex-grow:0;flex-shrink:1;flex-wrap:nowrap;float:none;font-family:initial;font-feature-settings:normal;font-kerning:auto;font-language-override:normal;font-size:medium;font-size-adjust:none;font-stretch:normal;font-style:normal;font-synthesis:weight style;font-variant:normal;font-variant-alternates:normal;font-variant-caps:normal;font-variant-east-asian:normal;font-variant-ligatures:normal;font-variant-numeric:normal;font-variant-position:normal;font-weight:400;grid-auto-columns:auto;grid-auto-flow:row;grid-auto-rows:auto;grid-column-end:auto;grid-column-gap:0;grid-column-start:auto;grid-row-end:auto;grid-row-gap:0;grid-row-start:auto;grid-template-areas:none;grid-template-columns:none;grid-template-rows:none;height:auto;hyphens:manual;image-orientation:0deg;image-rendering:auto;image-resolution:1dppx;ime-mode:auto;inline-size:auto;isolation:auto;justify-content:flexStart;left:auto;letter-spacing:normal;line-break:auto;line-height:normal;list-style-image:none;list-style-position:outside;list-style-type:disc;margin-block-end:0;margin-block-start:0;margin-bottom:0;margin-inline-end:0;margin-inline-start:0;margin-left:0;margin-right:0;margin-top:0;mask-clip:borderBox;mask-composite:add;mask-image:none;mask-mode:matchSource;mask-origin:borderBox;mask-position:0 0;mask-repeat:repeat;mask-size:auto;mask-type:luminance;max-height:none;max-width:none;min-block-size:0;min-height:0;min-inline-size:0;min-width:0;mix-blend-mode:normal;object-fit:fill;object-position:50% 50%;offset-block-end:auto;offset-block-start:auto;offset-inline-end:auto;offset-inline-start:auto;opacity:1;order:0;orphans:2;outline-color:initial;outline-offset:0;outline-style:none;outline-width:medium;overflow:visible;overflow-wrap:normal;overflow-x:visible;overflow-y:visible;padding-block-end:0;padding-block-start:0;padding-bottom:0;padding-inline-end:0;padding-inline-start:0;padding-left:0;padding-right:0;padding-top:0;page-break-after:auto;page-break-before:auto;page-break-inside:auto;perspective:none;perspective-origin:50% 50%;pointer-events:auto;position:static;quotes:initial;resize:none;right:auto;ruby-align:spaceAround;ruby-merge:separate;ruby-position:over;scroll-behavior:auto;scroll-snap-coordinate:none;scroll-snap-destination:0 0;scroll-snap-points-x:none;scroll-snap-points-y:none;scroll-snap-type:none;shape-image-threshold:0;shape-margin:0;shape-outside:none;tab-size:8;table-layout:auto;text-align:initial;text-align-last:auto;text-combine-upright:none;text-decoration-color:currentcolor;text-decoration-line:none;text-decoration-style:solid;text-emphasis-color:currentcolor;text-emphasis-position:over right;text-emphasis-style:none;text-indent:0;text-justify:auto;text-orientation:mixed;text-overflow:clip;text-rendering:auto;text-shadow:none;text-transform:none;text-underline-position:auto;top:auto;touch-action:auto;transform:none;transform-box:borderBox;transform-origin:50% 50%0;transform-style:flat;transition-delay:0s;transition-duration:0s;transition-property:all;transition-timing-function:ease;vertical-align:baseline;visibility:visible;white-space:normal;widows:2;width:auto;will-change:auto;word-break:normal;word-spacing:normal;word-wrap:normal;writing-mode:horizontalTb;z-index:auto;-webkit-appearance:none;-moz-appearance:none;-ms-appearance:none;appearance:none;margin:0}.LiveAreaSection-193358632{width:100%}.LiveAreaSection-193358632 .login-option-buybox{display:block;width:100%;font-size:17px;line-height:30px;color:#222;padding-top:30px;font-family:Harding,Palatino,serif}.LiveAreaSection-193358632 .additional-access-options{display:block;font-weight:700;font-size:17px;line-height:30px;color:#222;font-family:Harding,Palatino,serif}.LiveAreaSection-193358632 .additional-login>li:not(:first-child)::before{transform:translateY(-50%);content:””;height:1rem;position:absolute;top:50%;left:0;border-left:2px solid #999}.LiveAreaSection-193358632 .additional-login>li:not(:first-child){padding-left:10px}.LiveAreaSection-193358632 .additional-login>li{display:inline-block;position:relative;vertical-align:middle;padding-right:10px}.BuyBoxSection-683559780{display:flex;flex-wrap:wrap;flex:1;flex-direction:row-reverse;margin:-30px -15px 0}.BuyBoxSection-683559780 .box-inner{width:100%;height:100%}.BuyBoxSection-683559780 .readcube-buybox{background-color:#f3f3f3;flex-shrink:1;flex-grow:1;flex-basis:255px;background-clip:content-box;padding:0 15px;margin-top:30px}.BuyBoxSection-683559780 .subscribe-buybox{background-color:#f3f3f3;flex-shrink:1;flex-grow:4;flex-basis:300px;background-clip:content-box;padding:0 15px;margin-top:30px}.BuyBoxSection-683559780 .subscribe-buybox-nature-plus{background-color:#f3f3f3;flex-shrink:1;flex-grow:4;flex-basis:100%;background-clip:content-box;padding:0 15px;margin-top:30px}.BuyBoxSection-683559780 .title-readcube,.BuyBoxSection-683559780 .title-buybox{display:block;margin:0;margin-right:10%;margin-left:10%;font-size:24px;line-height:32px;color:#222;padding-top:30px;text-align:center;font-family:Harding,Palatino,serif}.BuyBoxSection-683559780 .title-asia-buybox{display:block;margin:0;margin-right:5%;margin-left:5%;font-size:24px;line-height:32px;color:#222;padding-top:30px;text-align:center;font-family:Harding,Palatino,serif}.BuyBoxSection-683559780 .asia-link{color:#069;cursor:pointer;text-decoration:none;font-size:1.05em;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif;line-height:1.05em6}.BuyBoxSection-683559780 .access-readcube{display:block;margin:0;margin-right:10%;margin-left:10%;font-size:14px;color:#222;padding-top:10px;text-align:center;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif;line-height:20px}.BuyBoxSection-683559780 .access-asia-buybox{display:block;margin:0;margin-right:5%;margin-left:5%;font-size:14px;color:#222;padding-top:10px;text-align:center;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif;line-height:20px}.BuyBoxSection-683559780 .access-buybox{display:block;margin:0;margin-right:10%;margin-left:10%;font-size:14px;color:#222;opacity:.8px;padding-top:10px;text-align:center;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif;line-height:20px}.BuyBoxSection-683559780 .price-buybox{display:block;font-size:30px;color:#222;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif;padding-top:30px;text-align:center}.BuyBoxSection-683559780 .price-buybox-to{display:block;font-size:30px;color:#222;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif;text-align:center}.BuyBoxSection-683559780 .price-info-text{font-size:16px;padding-right:10px;color:#222;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif}.BuyBoxSection-683559780 .price-value{font-size:30px;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif}.BuyBoxSection-683559780 .price-per-period{font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif}.BuyBoxSection-683559780 .price-from{font-size:14px;padding-right:10px;color:#222;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif;line-height:20px}.BuyBoxSection-683559780 .issue-buybox{display:block;font-size:13px;text-align:center;color:#222;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif;line-height:19px}.BuyBoxSection-683559780 .no-price-buybox{display:block;font-size:13px;line-height:18px;text-align:center;padding-right:10%;padding-left:10%;padding-bottom:20px;padding-top:30px;color:#222;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif}.BuyBoxSection-683559780 .vat-buybox{display:block;margin-top:5px;margin-right:20%;margin-left:20%;font-size:11px;color:#222;padding-top:10px;padding-bottom:15px;text-align:center;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif;line-height:17px}.BuyBoxSection-683559780 .tax-buybox{display:block;width:100%;color:#222;padding:20px 16px;text-align:center;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif;line-height:NaNpx}.BuyBoxSection-683559780 .button-container{display:flex;padding-right:20px;padding-left:20px;justify-content:center}.BuyBoxSection-683559780 .button-container>*{flex:1px}.BuyBoxSection-683559780 .button-container>a:hover,.Button-505204839:hover,.Button-1078489254:hover,.Button-2496381730:hover{text-decoration:none}.BuyBoxSection-683559780 .readcube-button{background:#fff;margin-top:30px}.BuyBoxSection-683559780 .button-asia{background:#069;border:1px solid #069;border-radius:0;cursor:pointer;display:block;padding:9px;outline:0;text-align:center;text-decoration:none;min-width:80px;margin-top:75px}.BuyBoxSection-683559780 .button-label-asia,.ButtonLabel-3869432492,.ButtonLabel-3296148077,.ButtonLabel-1651148777{display:block;color:#fff;font-size:17px;line-height:20px;font-family:-apple-system,BlinkMacSystemFont,”Segoe UI”,Roboto,Oxygen-Sans,Ubuntu,Cantarell,”Helvetica Neue”,sans-serif;text-align:center;text-decoration:none;cursor:pointer}.Button-505204839,.Button-1078489254,.Button-2496381730{background:#069;border:1px solid #069;border-radius:0;cursor:pointer;display:block;padding:9px;outline:0;text-align:center;text-decoration:none;min-width:80px;max-width:320px;margin-top:10px}.Button-505204839 .readcube-label,.Button-1078489254 .readcube-label,.Button-2496381730 .readcube-label{color:#069}
/* style specs end */
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Rent or buy this article
Prices vary by article type
from$1.95
to$39.95
Prices may be subject to local taxes which are calculated during checkout



References
-
Butler, M. S. et al. Analysis of the clinical pipeline of treatments for drug-resistant bacterial infections: despite progress, more action is needed. Antimicrob. Agents Chemother. 66, e0199121 (2022).
Google Scholar
-
Martínez-García, L., González-Alba, J. M., Baquero, F., Cantón, R. & Galán, J. C. Ceftazidime is the key diversification and selection driver of VIM-type carbapenemases. mBio 9, e02109–e02117 (2018).
Google Scholar
-
Baquero, F. et al. Allogenous selection of mutational collateral resistance: old drugs select for new resistance within antibiotic families. Front. Microbiol. 12, 757833 (2021).
Google Scholar
-
Rajer, F., Allander, L., Karlsson, P. A. & Sandegren, L. Evolutionary trajectories toward high-level β-lactam/β-lactamase inhibitor resistance in the presence of multiple β-lactamases. Antimicrob. Agents Chemother. 66, e0029022 (2022).
Google Scholar
-
Poirel, L., Sadek, M., Kusaksizoglu, A. & Nordmann, P. Co-resistance to ceftazidime–avibactam and cefiderocol in clinical isolates producing KPC variants. Eur. J. Clin. Microbiol. Infect. Dis. 41, 677–680 (2022).
Google Scholar
-
Silver, L. L. Challenges of antibacterial discovery. Clin. Microbiol. Rev. 24, 71–109 (2011).
Google Scholar
-
Baker, S. J., Payne, D. J., Rappuoli, R. & De Gregorio, E. Technologies to address antimicrobial resistance. Proc. Natl Acad. Sci. USA 115, 12887–12895 (2018).
Google Scholar
-
Payne, D. J., Gwynn, M. N., Holmes, D. J. & Pompliano, D. L. Drugs for bad bugs: confronting the challenges of antibacterial discovery. Nat. Rev. Drug Discov. 6, 29–40 (2007).
Google Scholar
-
Tommasi, R., Brown, D. G., Walkup, G. K., Manchester, J. I. & Miller, A. A. ESKAPEing the labyrinth of antibacterial discovery. Nat. Rev. Drug Discov. 14, 529–542 (2015).
Google Scholar
-
Brotz-Oesterhelt, H. & Sass, P. Postgenomic strategies in antibacterial drug discovery. Future Microbiol. 5, 1553–1579 (2010).
Google Scholar
-
Lewis, K. Platforms for antibiotic discovery. Nat. Rev. Drug Discov. 12, 371–387 (2013).
Google Scholar
-
Muñoz, K. A. & Hergenrother, P. J. Facilitating compound entry as a means to discover antibiotics for Gram-negative bacteria. Acc. Chem. Res. 54, 1322–1333 (2021).
Google Scholar
-
Zhao, S. et al. Defining new chemical space for drug penetration into Gram-negative bacteria. Nat. Chem. Biol. 16, 1293–1302 (2020).
Google Scholar
-
Sadybekov, A. V. & Katritch, V. Computational approaches streamlining drug discovery. Nature 616, 673–685 (2023).
Google Scholar
-
Lluka, T. & Stokes, J. M. Antibiotic discovery in the artificial intelligence era. Ann. NY Acad. Sci. 1519, 74–93 (2023).
Google Scholar
-
Lyu, J. et al. Ultra-large library docking for discovering new chemotypes. Nature 566, 224–229 (2019).
Google Scholar
-
Mobegi, F. M. et al. From microbial gene essentiality to novel antimicrobial drug targets. BMC Genomics 15, 958 (2014).
Google Scholar
-
Agarwal, P. & Searls, D. B. Can literature analysis identify innovation drivers in drug discovery? Nat. Rev. Drug Discov. 8, 865 (2009).
Google Scholar
-
Lange, R. P., Locher, H. H., Wyss, P. C. & Then, R. L. The targets of currently used antibacterial agents: lessons for drug discovery. Curr. Pharm. Des. 13, 3140–3154 (2007).
Google Scholar
-
Theuretzbacher, U. & Piddock, L. J. V. Non-traditional antibacterial therapeutic options and challenges. Cell Host Microbe 26, 61–72 (2019).
Google Scholar
-
Frearson, J. A., Wyatt, P. G., Gilbert, I. H. & Fairlamb, A. H. Target assessment for antiparasitic drug discovery. Trends Parasitol. 23, 589–595 (2007).
Google Scholar
-
Streker, K. et al. In vitro and in vivo validation of ligA and tarI as essential targets in Staphylococcus aureus. Antimicrob. Agents Chemother. 52, 4470–4474 (2008).
Google Scholar
-
Rancati, G., Moffat, J., Typas, A. & Pavelka, N. Emerging and evolving concepts in gene essentiality. Nat. Rev. Genet. 19, 34–49 (2018).
Google Scholar
-
Bosch-Guiteras, N. & van Leeuwen, J. Exploring conditional gene essentiality through systems genetics approaches in yeast. Curr. Opin. Genet. Dev. 76, 101963 (2022).
Google Scholar
-
Zhang, Z. & Ren, Q. Why are essential genes essential? – the essentiality of Saccharomyces genes. Microb. Cell 2, 280–287 (2015).
Google Scholar
-
Chessher, A. Evaluating the suitability of essential genes as targets for antibiotic screening assays using proteomics. Protein Cell 3, 5–7 (2012).
Google Scholar
-
Editorial. Putting gene essentiality into context. Nat. Rev. Genet. 19, 1 (2017).
-
Chaudhary, A. S., Chen, W., Jin, J., Tai, P. C. & Wang, B. SecA: a potential antimicrobial target. Future Med. Chem. 7, 989–1007 (2015).
Google Scholar
-
Emmerich, C. H. et al. Improving target assessment in biomedical research: the GOT-IT recommendations. Nat. Rev. Drug Discov. 20, 64–81 (2021).
Google Scholar
-
Murima, P., McKinney, J. D. & Pethe, K. Targeting bacterial central metabolism for drug development. Chem. Biol. 21, 1423–1432 (2014).
Google Scholar
-
Hedstrom, L. The bare essentials of antibiotic target validation. ACS Infect. Dis. 3, 2–4 (2017).
Google Scholar
-
Hogan, A. M. & Cardona, S. T. Gradients in gene essentiality reshape antibacterial research. FEMS Microbiol. Rev. 46, fuac005 (2022).
Google Scholar
-
Bergmiller, T., Ackermann, M. & Silander, O. K. Patterns of evolutionary conservation of essential genes correlate with their compensability. PLoS Genet. 8, e1002803 (2012).
Google Scholar
-
Dunman, P. M. & Tomaras, A. P. Translational deficiencies in antibacterial discovery and new screening paradigms. Curr. Opin. Microbiol. 27, 108–113 (2015).
Google Scholar
-
Rosconi, F. et al. A bacterial pan-genome makes gene essentiality strain-dependent and evolvable. Nat. Microbiol. 7, 1580–1592 (2022).
Google Scholar
-
Kaur, H., Kalia, M. & Taneja, N. Identification of novel non-homologous drug targets against Acinetobacter baumannii using subtractive genomics and comparative metabolic pathway analysis. Microb. Pathog. 152, 104608 (2021).
Google Scholar
-
Uddin, R., Masood, F., Azam, S. S. & Wadood, A. Identification of putative non-host essential genes and novel drug targets against Acinetobacter baumannii by in silico comparative genome analysis. Microb. Pathog. 128, 28–35 (2019).
Google Scholar
-
Ramos, P. I. P. et al. An integrative, multi-omics approach towards the prioritization of Klebsiella pneumoniae drug targets. Sci. Rep. 8, 10755 (2018).
Google Scholar
-
Rafiq, H. et al. A computational subtractive genome analysis for the characterization of novel drug targets in Klebsiella pneumoniae strain PittNDM01. Microb. Pathog. 146, 104245 (2020).
Google Scholar
-
Uddin, R. & Jamil, F. Prioritization of potential drug targets against P. aeruginosa by core proteomic analysis using computational subtractive genomics and protein–protein interaction network. Comput. Biol. Chem. 74, 115–122 (2018).
Google Scholar
-
Nazarshodeh, E., Marashi, S. A. & Gharaghani, S. Structural systems pharmacology: a framework for integrating metabolic network and structure-based virtual screening for drug discovery against bacteria. PLoS ONE 16, e0261267 (2021).
Google Scholar
-
Bakheet, T. M. & Doig, A. J. Properties and identification of antibiotic drug targets. BMC Bioinformatics 11, 195 (2010).
Google Scholar
-
Bosch, B. et al. Genome-wide gene expression tuning reveals diverse vulnerabilities of M. tuberculosis. Cell 184, 4579–4592.e24 (2021).
Google Scholar
-
Hawkins, J. S. et al. Mismatch-CRISPRi reveals the co-varying expression–fitness relationships of essential genes in Escherichia coli and Bacillus subtilis. Cell Syst. 11, 523–535.e9 (2020).
Google Scholar
-
Luo, H., Gao, F. & Lin, Y. Evolutionary conservation analysis between the essential and nonessential genes in bacterial genomes. Sci. Rep. 5, 13210 (2015).
Google Scholar
-
Arun, P. V. P. S. et al. Identification and functional analysis of essential, conserved, housekeeping and duplicated genes. FEBS Lett. 590, 1428–1437 (2016).
Google Scholar
-
Du, W. et al. Two active forms of UDP-N-acetylglucosamine enolpyruvyl transferase in Gram-positive bacteria. J. Bacteriol. 182, 4146–4152 (2000).
Google Scholar
-
Naz, S., Ngo, T., Farooq, U. & Abagyan, R. Analysis of drug binding pockets and repurposing opportunities for twelve essential enzymes of ESKAPE pathogens. PeerJ 5, e3765–e3765 (2017).
Google Scholar
-
Klahn, P. & Bronstrup, M. New structural templates for clinically validated and novel targets in antimicrobial drug research and development. Curr. Top. Microbiol. Immunol. 398, 365–417 (2016).
Google Scholar
-
Miranda, R. R., Parthasarathy, A. & Hudson, A. O. Exploration of chemical biology approaches to facilitate the discovery and development of novel antibiotics. Front. Trop. Dis. 3, 845469 (2022).
Google Scholar
-
Silver, L. L. A gestalt approach to Gram-negative entry. Bioorg. Med. Chem. 24, 6379–6389 (2016).
Google Scholar
-
Yu, N. Y., Laird, M. R., Spencer, C. & Brinkman, F. S. PSORTdb — an expanded, auto-updated, user-friendly protein subcellular localization database for Bacteria and Archaea. Nucleic Acids Res. 39, D241–D244 (2011).
Google Scholar
-
Agoni, C., Olotu, F. A., Ramharack, P. & Soliman, M. E. Druggability and drug-likeness concepts in drug design: are biomodelling and predictive tools having their say? J. Mol. Model. 26, 120 (2020).
Google Scholar
-
Vukovic, S. & Huggins, D. J. Quantitative metrics for drug-target ligandability. Drug Discov. Today 23, 1258–1266 (2018).
Google Scholar
-
Sheridan, R. P., Maiorov, V. N., Holloway, M. K., Cornell, W. D. & Gao, Y.-D. Drug-like density: a method of quantifying the “bindability” of a protein target based on a very large set of pockets and drug-like ligands from the protein data bank. J. Chem. Inf. Model. 50, 2029–2040 (2010).
Google Scholar
-
Paananen, J. & Fortino, V. An omics perspective on drug target discovery platforms. Brief. Bioinform. 21, 1937–1953 (2020).
Google Scholar
-
Coyle, J. & Walser, R. Applied biophysical methods in fragment-based drug discovery. SLAS Discov. 25, 471–490 (2020).
Google Scholar
-
Jumper, J. et al. Highly accurate protein structure prediction with AlphaFold. Nature 596, 583–589 (2021).
Google Scholar
-
Canning, P., Birchall, K., Kettleborough, C. A., Merritt, A. & Coombs, P. J. Fragment-based target screening as an empirical approach to prioritising targets: a case study on antibacterials. Drug Discov. Today 25, 2030–2037 (2020).
Google Scholar
-
Machutta, C. A. et al. Prioritizing multiple therapeutic targets in parallel using automated DNA-encoded library screening. Nat. Commun. 8, 16081 (2017).
Google Scholar
-
Sutterlin, H. A., Malinverni, J. C., Lee, S. H., Balibar, C. J. & Roemer, T. in Antibacterials Vol.1 (eds Fisher, J. F., Mobashery, S. & Miller, M. J.) 1–29 (Springer, 2018).
-
Serral, F. et al. From genome to drugs: new approaches in antimicrobial discovery. Front. Pharmacol. 12, 647060 (2021).
Google Scholar
-
Privalsky, T. M. et al. Prospects for antibacterial discovery and development. J. Am. Chem. Soc. 143, 21127–21142 (2021).
Google Scholar
-
Lin, Z. et al. Evolutionary-scale prediction of atomic level protein structure with a language model. Science 379, 1123–1130 (2023).
Google Scholar
-
Wua, R. et al. High-resolution de novo structure prediction from primary sequence. Preprint at bioRxiv https://doi.org/10.1101/2022.07.21.500999 (2022).
-
Suárez-Rivero, J. M. et al. Mitochondria and antibiotics: for good or for evil? Biomolecules 11, 1050 (2021).
Google Scholar
-
Hoogstraten, C. A., Lyon, J. J., Smeitink, J. A. M., Russel, F. G. M. & Schirris, T. J. J. Time to change: a systems pharmacology approach to disentangle mechanisms of drug-induced mitochondrial toxicity. Pharmacol. Rev. 75, 463–486 (2023).
Google Scholar
-
Darby, E. M. et al. Molecular mechanisms of antibiotic resistance revisited. Nat. Rev. Microbiol. 21, 280–295 (2023).
Google Scholar
-
Lewis, K. The science of antibiotic discovery. Cell 181, 29–45 (2020).
Google Scholar
-
Silver, L. L. Appropriate targets for antibacterial drugs. Cold Spring Harb. Perspect. Med. 6, a030239 (2016).
Google Scholar
-
O’Dwyer, K. et al. Bacterial resistance to leucyl-tRNA synthetase inhibitor GSK2251052 develops during treatment of complicated urinary tract infections. Antimicrob. Agents Chemother. 59, 289–298 (2015).
Google Scholar
-
Purnapatre, K. P. et al. In vitro and in vivo activities of DS86760016, a novel leucyl-tRNA synthetase inhibitor for Gram-negative pathogens. Antimicrob. Agents Chemother. 62, e01987-17 (2018).
Google Scholar
-
Min, S. et al. Frequency of spontaneous resistance to peptide deformylase inhibitor GSK1322322 in Haemophilus influenzae, Staphylococcus aureus, Streptococcus pyogenes, and Streptococcus pneumoniae. Antimicrob. Agents Chemother. 59, 4644–4652 (2015).
Google Scholar
-
Apfel, C. M. et al. Peptide deformylase as an antibacterial drug target: target validation and resistance development. Antimicrob. Agents Chemother. 45, 1058–1064 (2001).
Google Scholar
-
Redgrave, L. S., Sutton, S. B., Webber, M. A. & Piddock, L. J. V. Fluoroquinolone resistance: mechanisms, impact on bacteria, and role in evolutionary success. Trends Microbiol. 22, 438–445 (2014).
Google Scholar
-
Silver, L. L. Multi-targeting by monotherapeutic antibacterials. Nat. Rev. Drug Discov. 6, 41–55 (2007).
Google Scholar
-
Martin, J. K. II et al. A dual-mechanism antibiotic kills Gram-negative bacteria and avoids drug resistance. Cell 181, 1518–1532 e14 (2020).
Google Scholar
-
Theuretzbacher, U. Dual-mechanism antibiotics. Nat. Microbiol. 5, 984–985 (2020).
Google Scholar
-
Liu, D. Y. et al. Collateral sensitivity profiling in drug-resistant Escherichia coli identifies natural products suppressing cephalosporin resistance. Nat. Commun. 14, 1976 (2023).
Google Scholar
-
Caveney, N. A. et al. Structural insight into YcbB-mediated beta-lactam resistance in Escherichia coli. Nat. Commun. 10, 1849 (2019).
Google Scholar
-
Moradigaravand, D. et al. Prediction of antibiotic resistance in Escherichia coli from large-scale pan-genome data. PLoS Comput. Biol. 14, e1006258 (2018).
Google Scholar
-
Zgurskaya, H. I. & Rybenkov, V. V. Permeability barriers of Gram-negative pathogens. Ann. NY Acad. Sci. 1459, 5–18 (2020).
Google Scholar
-
Walker, S. S. & Black, T. A. Are outer-membrane targets the solution for MDR Gram-negative bacteria? Drug Discov. Today 26, 2152–2158 (2021).
Google Scholar
-
Raetz, C. R. et al. Discovery of new biosynthetic pathways: the lipid A story. J. Lipid Res. 50, S103–S108 (2009).
Google Scholar
-
Lehman, K. M. & Grabowicz, M. Countering Gram-negative antibiotic resistance: recent progress in disrupting the outer membrane with novel therapeutics. Antibiotics 8, 163 (2019).
Google Scholar
-
Horne, J. E., Brockwell, D. J. & Radford, S. E. Role of the lipid bilayer in outer membrane protein folding in Gram-negative bacteria. J. Biol. Chem. 295, 10340–10367 (2020).
Google Scholar
-
Choi, U. & Lee, C. R. Antimicrobial agents that inhibit the outer membrane assembly machines of Gram-negative bacteria. J. Microbiol. Biotechnol. 29, 1–10 (2019).
Google Scholar
-
Kovacs-Simon, A., Titball, R. W. & Michell, S. L. Lipoproteins of bacterial pathogens. Infect. Immun. 79, 548–561 (2011).
Google Scholar
-
Li, Y. et al. Identification of a compound that inhibits the growth of Gram-negative bacteria by blocking BamA–BamD interaction. Front. Microbiol. 11, 1252 (2020).
Google Scholar
-
Ghequire, M. G. K., Swings, T., Michiels, J., Buchanan, S. K. & De Mot, R. Hitting with a BAM: selective killing by lectin-like bacteriocins. mBio 9, e02138-17 (2018).
Google Scholar
-
Storek, K. M. et al. Monoclonal antibody targeting the β-barrel assembly machine of Escherichia coli is bactericidal. Proc. Natl Acad. Sci. USA 115, 3692–3697 (2018).
Google Scholar
-
Robinson, J. A. Folded synthetic peptides and other molecules targeting outer membrane protein complexes in Gram-negative bacteria. Front. Chem. 7, 45 (2019).
Google Scholar
-
Hart, E. M. et al. A small-molecule inhibitor of BamA impervious to efflux and the outer membrane permeability barrier. Proc. Natl Acad. Sci. USA 116, 21748–21757 (2019).
Google Scholar
-
Wade, N. et al. Synthesis and structure–activity studies of β-barrel assembly machine complex inhibitor MRL-494. ACS Infect. Dis. 8, 2242–2252 (2022).
Google Scholar
-
Imai, Y. et al. A new antibiotic selectively kills Gram-negative pathogens. Nature 576, 459–464 (2019).
Google Scholar
-
Kaur, H. et al. The antibiotic darobactin mimics a β-strand to inhibit outer membrane insertase. Nature 593, 125–129 (2021).
Google Scholar
-
Miller, R. D. et al. Computational identification of a systemic antibiotic for Gram-negative bacteria. Nat. Microbiol. 7, 1661–1672 (2022).
Google Scholar
-
Luther, A. et al. Chimeric peptidomimetic antibiotics against Gram-negative bacteria. Nature 576, 452–458 (2019).
Google Scholar
-
Groß, S. et al. Improved broad-spectrum antibiotics against Gram-negative pathogens via darobactin biosynthetic pathway engineering. Chem. Sci. 12, 11882–11893 (2021).
Google Scholar
-
Wuisan, Z. G., Kresna, I. D. M., Bohringer, N., Lewis, K. & Schaberle, T. F. Optimization of heterologous darobactin A expression and identification of the minimal biosynthetic gene cluster. Metab. Eng. 66, 123–136 (2021).
Google Scholar
-
Seyfert, C. E. et al. Darobactins exhibiting superior antibiotic activity by cryo-EM structure guided biosynthetic engineering. Angew. Chem. Int. Ed. 62, e202214094 (2023).
Google Scholar
-
Steenhuis, M. et al. Combining cell envelope stress reporter assays in a screening approach to identify BAM complex inhibitors. ACS Infect. Dis. 7, 2250–2263 (2021).
Google Scholar
-
Kaushik, S., He, H. & Dalbey, R. E. Bacterial signal peptides – navigating the journey of proteins. Front. Physiol. 13, 933153 (2022).
Google Scholar
-
Rao, C. V. S., De Waelheyns, E., Economou, A. & Anné, J. Antibiotic targeting of the bacterial secretory pathway. Biochim. Biophys. Acta 1843, 1762–1783 (2014).
Google Scholar
-
Ambroziak, P., Rzepka, I. & Skorko-Glonek, J. SecA – a multidomain and multitask bacterial export protein. Acta Biochim. Pol. 68, 427–436 (2021).
Google Scholar
-
De Waelheyns, E. et al. Identification of small-molecule inhibitors against SecA by structure-based virtual ligand screening. J. Antibiot. 68, 666–673 (2015).
Google Scholar
-
Jin, J. et al. SecA inhibitors as potential antimicrobial agents: differential actions on SecA-only and SecA–SecYEG protein-conducting channels. FEMS Microbiol. Lett. 365, fny145 (2018).
Google Scholar
-
Alksne, L. E. et al. Identification and analysis of bacterial protein secretion inhibitors utilizing a SecA–LacZ reporter fusion system. Antimicrob. Agents Chemother. 44, 1418–1427 (2000).
Google Scholar
-
Seinen, A.-B., Spakman, D., van Oijen, A. M. & Driessen, A. J. M. Cellular dynamics of the SecA ATPase at the single molecule level. Sci. Rep. 11, 1433 (2021).
Google Scholar
-
Braunstein, M., Bensing, B. A. & Sullam, P. M. The two distinct types of SecA2-dependent export systems. Microbiol. Spectr. 7, https://doi.org/10.1128/microspec.PSIB-0025-2018 (2019).
-
Jin, J. et al. Using chemical probes to assess the feasibility of targeting SecA for developing antimicrobial agents against Gram-negative bacteria. ChemMedChem 11, 2511–2521 (2016).
Google Scholar
-
Segers, K. & Anné, J. Traffic jam at the bacterial sec translocase: targeting the SecA nanomotor by small-molecule inhibitors. Chem. Biol. 18, 685–698 (2011).
Google Scholar
-
Dalbey, R. E., Lively, M. O., Bron, S. & van Dijl, J. M. The chemistry and enzymology of the type I signal peptidases. Protein Sci. 6, 1129–1138 (1997).
Google Scholar
-
Auclair, S. M., Bhanu, M. K. & Kendall, D. A. Signal peptidase I: cleaving the way to mature proteins. Protein Sci. 21, 13–25 (2012).
Google Scholar
-
Personne, Y., Curtis, M. A., Wareham, D. W. & Waite, R. D. Activity of the type I signal peptidase inhibitor MD3 against multidrug-resistant Gram-negative bacteria alone and in combination with colistin. J. Antimicrob. Chemother. 69, 3236–3243 (2014).
Google Scholar
-
De Rosa, M. et al. Design, synthesis and in vitro biological evaluation of oligopeptides targeting E. coli type I signal peptidase (LepB). Bioorg. Med. Chem. 25, 897–911 (2017).
Google Scholar
-
Smith, P. A. & Romesberg, F. E. Mechanism of action of the arylomycin antibiotics and effects of signal peptidase I inhibition. Antimicrob. Agents Chemother. 56, 5054–5060 (2012).
Google Scholar
-
Barbosa, M. D. F. S. et al. Regulated expression of the Escherichia coli lepB gene as a tool for cellular testing of antimicrobial compounds that inhibit signal peptidase i in vitro. Antimicrob. Agents Chemother. 46, 3549–3554 (2002).
Google Scholar
-
Craney, A. & Romesberg, F. E. The inhibition of type I bacterial signal peptidase: biological consequences and therapeutic potential. Bioorg. Med. Chem. Lett. 25, 4761–4766 (2015).
Google Scholar
-
Therien, A. G. et al. Broadening the spectrum of beta-lactam antibiotics through inhibition of signal peptidase type I. Antimicrob. Agents Chemother. 56, 4662–4670 (2012).
Google Scholar
-
Gao, M., Nakajima, A. D. & Skolnick, J. Deep learning-driven insights into super protein complexes for outer membrane protein biogenesis in bacteria. eLife 11, e82885 (2022).
Google Scholar
-
Smith, P. A. et al. Optimized arylomycins are a new class of Gram-negative antibiotics. Nature 561, 189–194 (2018).
Google Scholar
-
Girgis, H. S. et al. Single-molecule nanopore sequencing reveals extreme target copy number heterogeneity in arylomycin-resistant mutants. Proc. Natl Acad. Sci. USA 118, e2021958118 (2021).
Google Scholar
-
Bhaskar, B. V. et al. Structure-based virtual screening of Pseudomonas aeruginosa LpxA inhibitors using pharmacophore-based approach. Biomolecules 10, 266 (2020).
Google Scholar
-
Sacco, M. D. et al. Structure-based ligand design targeting Pseudomonas aeruginosa LpxA in lipid A biosynthesis. ACS Infect. Dis. 8, 1231–1240 (2022).
Google Scholar
-
Ma, X. et al. Structural and biological basis of small molecule inhibition of Escherichia coli LpxD acyltransferase essential for lipopolysaccharide biosynthesis. ACS Infect. Dis. 6, 1480–1489 (2020).
Google Scholar
-
Badger, J. et al. Structure determination of LpxD from the lipopolysaccharide-synthesis pathway of Acinetobacter baumannii. Acta Crystallogr. F 69, 6–9 (2013).
Google Scholar
-
Mdluli, K. E. et al. Molecular validation of LpxC as an antibacterial drug target in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 50, 2178–2184 (2006).
Google Scholar
-
Ryan, M. D. et al. Discovery of novel UDP-N-Acetylglucosamine acyltransferase (LpxA) inhibitors with activity against Pseudomonas aeruginosa. J. Med. Chem. 64, 14377–14425 (2021).
Google Scholar
-
Erwin, A. L. Antibacterial drug discovery targeting the lipopolysaccharide biosynthetic enzyme LpxC. Cold Spring Harb. Perspect. Med. 6, ea025304 (2016).
Google Scholar
-
Zhou, P. & Hong, J. Structure- and ligand-dynamics-based design of novel antibiotics targeting lipid A enzymes LpxC and LpxH in Gram-negative bacteria. Acc. Chem. Res. 54, 1623–1634 (2021).
Google Scholar
-
Panchaud, P. et al. Optimization of LpxC inhibitor lead compounds focusing on efficacy and formulation for high dose intravenous administration. J. Med. Chem. 63, 88–102 (2020).
Google Scholar
-
Surivet, J. P. et al. Discovery of novel inhibitors of LpxC displaying potent in vitro activity against Gram-negative bacteria. J. Med. Chem. 63, 66–87 (2020).
Google Scholar
-
Krause, K. M. et al. Potent LpxC inhibitors with in vitro activity against multidrug-resistant Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 63, e00977–e01019 (2019).
Google Scholar
-
Cohen, F. et al. Optimization of LpxC inhibitors for antibacterial activity and cardiovascular safety. ChemMedChem 14, 1560–1572 (2019).
Google Scholar
-
Ahmad, S. et al. Subtractive genomics, molecular docking and molecular dynamics simulation revealed LpxC as a potential drug target against multi-drug resistant Klebsiella pneumoniae. Interdiscip. Sci. 11, 508–526 (2019).
Google Scholar
-
Tomaras, A. P. et al. LpxC inhibitors as new antibacterial agents and tools for studying regulation of lipid A biosynthesis in Gram-negative pathogens. mBio 5, e01551-14 (2014).
Google Scholar
-
Yamada, Y. et al. Fragment-based discovery of novel non-hydroxamate LpxC inhibitors with antibacterial activity. J. Med. Chem. 63, 14805–14820 (2020).
Google Scholar
-
Pal, S. K. & Kumar, S. LpxC (UDP-3-O-(R-3-hydroxymyristoyl)-N-acetylglucosamine deacetylase) inhibitors: a long path explored for potent drug design. Int. J. Biol. Macromol. 234, 122960 (2023).
Google Scholar
-
Yoshida, I., Takata, I., Fujita, K., Takashima, H. & Sugiyama, H. TP0586532, a novel non-hydroxamate LpxC inhibitor: potentiating effect on in vitro activity of meropenem against carbapenem-resistant Enterobacteriaceae. Microbiol. Spectr. 10, e0082822 (2022).
Google Scholar
-
Zoghlami, M., Oueslati, M., Basharat, Z., Sadfi-Zouaoui, N. & Messaoudi, A. Inhibitor assessment against the LpxC enzyme of antibiotic-resistant Acinetobacter baumannii using virtual screening, dynamics simulation, and in vitro assays. Mol. Inform. 42, e2200061 (2023).
Google Scholar
-
Furuya, T. et al. N-Hydroxyformamide LpxC inhibitors, their in vivo efficacy in a mouse Escherichia coli infection model, and their safety in a rat hemodynamic assay. Bioorg. Med. Chem. 28, 115826 (2020).
Google Scholar
-
Lin, L. et al. Inhibition of LpxC protects mice from resistant Acinetobacter baumannii by modulating inflammation and enhancing phagocytosis. mBio 3, e00312–e00412 (2012).
Google Scholar
-
Emiola, A., George, J. & Andrews, S. S. A complete pathway model for lipid a biosynthesis in Escherichia coli. PLoS ONE 10, e0121216 (2015).
Google Scholar
-
Jones, A. K. et al. Mutations reducing in vitro susceptibility to novel LpxC inhibitors in Pseudomonas aeruginosa and interplay of efflux and nonefflux mechanisms. Antimicrob. Agents Chemother. 64, 17–27 (2019).
Google Scholar
-
Niu, Z. et al. Small molecule LpxC inhibitors against Gram-negative bacteria: advances and future perspectives. Eur. J. Med. Chem. 253, 115326 (2023).
Google Scholar
-
Kroeck, K. G. et al. Discovery of dual-activity small-molecule ligands of Pseudomonas aeruginosa LpxA and LpxD using SPR and X-ray crystallography. Sci. Rep. 9, 15450 (2019).
Google Scholar
-
Han, W. et al. Two distinct mechanisms of inhibition of LpxA acyltransferase essential for lipopolysaccharide biosynthesis. J. Am. Chem. Soc. 142, 4445–4455 (2020).
Google Scholar
-
Nayar, A. S. et al. Novel antibacterial targets and compounds revealed by a high-throughput cell wall reporter assay. J. Bacteriol. 197, 1726–1734 (2015).
Google Scholar
-
Kwak, S. H. et al. Development of LpxH inhibitors chelating the active site dimanganese metal cluster of LpxH. ChemMedChem 18, e202300023 (2023).
Google Scholar
-
Bohl, T. E. et al. The substrate-binding cap of the UDP-diacylglucosamine pyrophosphatase LpxH is highly flexible, enabling facile substrate binding and product release. J. Biol. Chem. 293, 7969–7981 (2018).
Google Scholar
-
Bonifer, C. & Glaubitz, C. MsbA: an ABC transporter paradigm. Biochem. Soc. Trans. 49, 2917–2927 (2021).
Google Scholar
-
Gorzelak, P., Klein, G. & Raina, S. Molecular basis of essentiality of early critical steps in the lipopolysaccharide biogenesis in Escherichia coli K-12: requirement of MsbA, cardiolipin, LpxL, LpxM and GcvB. Int. J. Mol. Sci. 22, 5099 (2021).
Google Scholar
-
Becker, J. P., Depret, G., Van Bambeke, F., Tulkens, P. M. & Prévost, M. Molecular models of human P-glycoprotein in two different catalytic states. BMC Struct. Biol. 9, 3 (2009).
Google Scholar
-
Zhou, Z., White, K. A., Polissi, A., Georgopoulos, C. & Raetz, C. R. H. Function of Escherichia coli MsbA, an essential ABC family transporter, in lipid A and phospholipid biosynthesis. J. Biol. Chem. 273, 12466–12475 (1998).
Google Scholar
-
Ghanei, H., Abeyrathne, P. D. & Lam, J. S. Biochemical characterization of MsbA from Pseudomonas aeruginosa. J. Biol. Chem. 282, 26939–26947 (2007).
Google Scholar
-
Zhang, G. et al. Cell-based screen for discovering lipopolysaccharide biogenesis inhibitors. Proc. Natl Acad. Sci. USA 115, 6834–6839 (2018).
Google Scholar
-
Verma, V. A. et al. Discovery of inhibitors of the lipopolysaccharide transporter MsbA: from a screening hit to potent wild-type Gram-negative activity. J. Med. Chem. 65, 4085–4120 (2022).
Google Scholar
-
Ho, J. M., Bakkalbasi, E., Söll, D. & Miller, C. A. Drugging tRNA aminoacylation. RNA Biol. 15, 667–677 (2018).
Google Scholar
-
Alexander, M. K. et al. Disrupting Gram-negative bacterial outer membrane biosynthesis through inhibition of the lipopolysaccharide transporter MsbA. Antimicrob. Agents Chemother. 62, e01142-18 (2018).
Google Scholar
-
Moura, E. C. C. M. et al. Thanatin impairs lipopolysaccharide transport complex assembly by targeting LptC–LptA interaction and decreasing LptA stability. Front. Microbiol. 11, 909 (2020).
Google Scholar
-
Simpson, B. W. & Trent, M. S. Pushing the envelope: LPS modifications and their consequences. Nat. Rev. Microbiol. 17, 403–416 (2019).
Google Scholar
-
Hicks, G. & Jia, Z. Structural basis for the lipopolysaccharide export activity of the bacterial lipopolysaccharide transport system. Int. J. Mol. Sci. 19, 2680 (2018).
Google Scholar
-
Botos, I. et al. Structural and functional characterization of the LPS transporter LptDE from Gram-negative pathogens. Structure 24, 965–976 (2016).
Google Scholar
-
Storek, K. M. et al. Massive antibody discovery used to probe structure–function relationships of the essential outer membrane protein LptD. eLife 8, e46258 (2019).
Google Scholar
-
Martin-Loeches, I., Dale, G. E. & Torres, A. Murepavadin: a new antibiotic class in the pipeline. Expert Rev. Anti Infect. Ther. 16, 259–268 (2018).
Google Scholar
-
Wach, A., Dembowsky, K. & Dale, G. E. Pharmacokinetics and safety of intravenous murepavadin infusion in healthy adult subjects administered single and multiple ascending doses. Antimicrob. Agents Chemother. 62, e02355-17 (2018).
Google Scholar
-
Romano, K. P. et al. Mutations in pmrB confer cross-resistance between the LptD inhibitor POL7080 and colistin in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 63, e00511-19 (2019).
Google Scholar
-
Bollati, M. et al. Crystal structure of LptH, the periplasmic component of the lipopolysaccharide transport machinery from Pseudomonas aeruginosa. FEBS J. 282, 1980–1997 (2015).
Google Scholar
-
Fernández-Piñar, R. et al. In vitro and in vivo screening for novel essential cell-envelope proteins in Pseudomonas aeruginosa. Sci. Rep. 5, 17593 (2015).
Google Scholar
-
Sinha, S., Dhanabal, V. B., Sperandeo, P., Polissi, A. & Bhattacharjya, S. Linking dual mode of action of host defense antimicrobial peptide thanatin: structures, lipopolysaccharide and LptA(m) binding of designed analogs. Biochim. Biophys. Acta 1864, 183839 (2022).
Google Scholar
-
Dai, X. et al. Identification of a small molecule that inhibits the interaction of LPS transporters LptA and LptC. Antibiotics 11, 1385 (2022).
Google Scholar
-
Schuster, M. et al. Peptidomimetic antibiotics disrupt the lipopolysaccharide transport bridge of drug-resistant Enterobacteriaceae. Sci. Adv. 9, eadg3683 (2023).
Google Scholar
-
Dash, R. & Bhattacharjya, S. Thanatin: an emerging host defense antimicrobial peptide with multiple modes of action. Int. J. Mol. Sci. 22, 1–13 (2021).
Google Scholar
-
Oi, K. K., Moehle, K., Schuster, M. & Zerbe, O. Early molecular insights into thanatin analogues binding to A. baumannii LptA. Molecules 28, 4335 (2023).
Google Scholar
-
Konovalova, A., Kahne, D. E. & Silhavy, T. J. Outer membrane biogenesis. Annu. Rev. Microbiol. 71, 539–556 (2017).
Google Scholar
-
Narita, S. I. & Tokuda, H. Bacterial lipoproteins; biogenesis, sorting and quality control. Biochim. Biophys. Acta 1862, 1414–1423 (2017).
Google Scholar
-
Grabowicz, M. & Silhavy, T. J. Redefining the essential trafficking pathway for outer membrane lipoproteins. Proc. Natl Acad. Sci. USA 114, 4769–4774 (2017).
Google Scholar
-
Nickerson, N. N. et al. A novel inhibitor of the LolCDE ABC transporter essential for lipoprotein trafficking in Gram-negative bacteria. Antimicrob. Agents Chemother. 62, e02151-17 (2018).
Google Scholar
-
McLeod, S. M. et al. Small-molecule inhibitors of Gram-negative lipoprotein trafficking discovered by phenotypic screening. J. Bacteriol. 197, 1075–1082 (2015).
Google Scholar
-
Avis, T., Wilson, F. X., Khan, N., Mason, C. S. & Powell, D. J. Targeted microbiome-sparing antibiotics. Drug Discov. Today 26, 2198–2203 (2021).
Google Scholar
-
Diao, J. et al. Inhibition of Escherichia coli lipoprotein diacylglyceryl transferase is insensitive to resistance caused by deletion of Braun’s lipoprotein. J. Bacteriol. 203, e0014921 (2021).
Google Scholar
-
Vogeley, L. et al. Structural basis of lipoprotein signal peptidase II action and inhibition by the antibiotic globomycin. Science 351, 876–880 (2016).
Google Scholar
-
Xia, J. et al. Bacterial lipoprotein biosynthetic pathway as a potential target for structure-based design of antibacterial agents. Curr. Med. Chem. 27, 1132–1150 (2020).
Google Scholar
-
El Arnaout, T. & Soulimane, T. Targeting lipoprotein biogenesis: considerations towards antimicrobials. Trends Biochem. Sci. 44, 701–715 (2019).
Google Scholar
-
Caldwell, T. A., Vickery, O. N., Colburn, J. D., Stansfeld, P. J. & Columbus, L. Conformational dynamics of the membrane enzyme LspA upon antibiotic and substrate binding. Biophys. J. 121, 2078–2083 (2022).
Google Scholar
-
Kitamura, S., Owensby, A., Wall, D. & Wolan, D. W. Lipoprotein signal peptidase inhibitors with antibiotic properties identified through design of a robust in vitro HT platform. Cell Chem. Biol. 25, 301–308 e12 (2018).
Google Scholar
-
Garland, K. et al. Optimization of globomycin analogs as novel Gram-negative antibiotics. Bioorg. Med. Chem. Lett. 30, 127419 (2020).
Google Scholar
-
Pantua, H. et al. Unstable mechanisms of resistance to inhibitors of Escherichia coli lipoprotein signal peptidase. mBio 11, e02018–e02020 (2020).
Google Scholar
-
Sauvage, E. & Terrak, M. Glycosyltransferases and transpeptidases/penicillin-binding proteins: valuable targets for new antibacterials. Antibiotics 5, 12 (2016).
Google Scholar
-
Ostash, B. & Walker, S. Moenomycin family antibiotics: chemical synthesis, biosynthesis, and biological activity. Nat. Prod. Rep. 27, 1594–1617 (2010).
Google Scholar
-
Galley, N. F., O’Reilly, A. M. & Roper, D. I. Prospects for novel inhibitors of peptidoglycan transglycosylases. Bioorg. Chem. 55, 16–26 (2014).
Google Scholar
-
den Blaauwen, T., Andreu, J. M. & Monasterio, O. Bacterial cell division proteins as antibiotic targets. Bioorg. Chem. 55, 27–38 (2014).
Google Scholar
-
Mohammadi, T. et al. Identification of FtsW as a transporter of lipid-linked cell wall precursors across the membrane. EMBO J. 30, 1425–1432 (2011).
Google Scholar
-
Attaibi, M. & Den Blaauwen, T. An updated model of the divisome: regulation of the septal peptidoglycan synthesis machinery by the divisome. Int. J. Mol. Sci. 23, 3537 (2022).
Google Scholar
-
Park, Y., Taguchi, A., Baidin, V., Kahne, D. & Walker, S. A time-resolved FRET assay identifies a small molecule that inhibits the essential bacterial cell wall polymerase FtsW. Angew. Chem. Int. Ed. 62, e202301522 (2023).
Google Scholar
-
Hering, J., Dunevall, E., Ek, M. & Brändén, G. Structural basis for selective inhibition of antibacterial target MraY, a membrane-bound enzyme involved in peptidoglycan synthesis. Drug Discov. Today 23, 1426–1435 (2018).
Google Scholar
-
Kubra, K. T., Uddin, M. A. & Barabutis, N. Tunicamycin protects against LPS-induced lung injury. Pharmaceuticals 15, 134 (2022).
Google Scholar
-
Nakaya, T. et al. Synthesis of macrocyclic nucleoside antibacterials and their interactions with MraY. Nat. Commun. 13, 7575 (2022).
Google Scholar
-
Hakulinen, J. K. et al. MraY–antibiotic complex reveals details of tunicamycin mode of action. Nat. Chem. Biol. 13, 265–267 (2017).
Google Scholar
-
Mashalidis, E. H. et al. Chemical logic of MraY inhibition by antibacterial nucleoside natural products. Nat. Commun. 10, 2917 (2019).
Google Scholar
-
Ichikawa, S. Bridge between total synthesis of bioactive natural products and development of drug leads [Japanese]. Yakugaku Zasshi 142, 355–363 (2022).
Google Scholar
-
Silver, L. L. Viable screening targets related to the bacterial cell wall. Ann. NY Acad. Sci. 1277, 29–53 (2013).
Google Scholar
-
Amera, G. M. et al. Prioritization of Mur family drug targets against A. baumannii and identification of their homologous proteins through molecular phylogeny, primary sequence, and structural analysis. J. Genet. Eng. Biotechnol. 18, 33 (2020).
Google Scholar
-
Liang, H. et al. Elucidating the inhibition of peptidoglycan biosynthesis in Staphylococcus aureus by albocycline, a macrolactone isolated from Streptomyces maizeus. Bioorg. Med. Chem. 26, 3453–3460 (2018).
Google Scholar
-
Chang, C. M. et al. Avenaciolides: potential MurA-targeted inhibitors against peptidoglycan biosynthesis in methicillin-resistant Staphylococcus aureus (MRSA). J. Am. Chem. Soc. 137, 267–275 (2015).
Google Scholar
-
Hrast, M., Sosič, I., Sink, R. & Gobec, S. Inhibitors of the peptidoglycan biosynthesis enzymes MurA–F. Bioorg. Chem. 55, 2–15 (2014).
Google Scholar
-
Hamilton, D. J. et al. Bromo-cyclobutenaminones as new covalent UDP-N-acetylglucosamine enolpyruvyl transferase (MurA) inhibitors. Pharmaceuticals 13, 362 (2020).
Google Scholar
-
Gaur, V. & Bera, S. Recent developments on UDP-N-acetylmuramoyl-l-alanine-d-gutamate ligase (Mur D) enzyme for antimicrobial drug development: an emphasis on in-silico approaches. Curr. Res. Pharmacol. Drug Discov. 3, 100137 (2022).
Google Scholar
-
Kouidmi, I., Levesque, R. C. & Paradis-Bleau, C. The biology of Mur ligases as an antibacterial target. Mol. Microbiol. 94, 242–253 (2014).
Google Scholar
-
Jha, R. K. et al. Identification of promising molecules against MurD ligase from Acinetobacter baumannii: insights from comparative protein modelling, virtual screening, molecular dynamics simulations and MM/PBSA analysis. J. Mol. Model. 26, 304 (2020).
Google Scholar
-
Ranjan Sahoo, C. et al. Coumarin derivatives as promising antibacterial agent(s). Arab. J. Chem. 14, 102922 (2021).
Google Scholar
-
Lock, R. L. & Harry, E. J. Cell-division inhibitors: new insights for future antibiotics. Nat. Rev. Drug Discov. 7, 324–338 (2008).
Google Scholar
-
De Pereda, J. M., Leynadier, D., Evangelio, J. A., Chacón, P. & Andreu, J. M. Tubulin secondary structure analysis, limited proteolysis sites, and homology to FtsZ. Biochemistry 35, 14203–14215 (1996).
Google Scholar
-
Ohashi, Y. et al. The lethal effect of a benzamide derivative, 3-methoxybenzamide, can be suppressed by mutations within a cell division gene, ftsZ, in Bacillus subtilis. J. Bacteriol. 181, 1348–1351 (1999).
Google Scholar
-
Miguel, A. et al. Variations in the binding pocket of an inhibitor of the bacterial division protein FtsZ across genotypes and species. PLoS Comput. Biol. 11, e1004117 (2015).
Google Scholar
-
Kaul, M. et al. TXA709, an FtsZ-targeting benzamide prodrug with improved pharmacokinetics and enhanced in vivo efficacy against methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 59, 4845–4855 (2015).
Google Scholar
-
Stokes, N. R. et al. Design, synthesis and structure-activity relationships of substituted oxazole-benzamide antibacterial inhibitors of FtsZ. Bioorg. Med. Chem. Lett. 24, 353–359 (2014).
Google Scholar
-
Fujita, J. et al. Structural flexibility of an inhibitor overcomes drug resistance mutations in Staphylococcus aureus FtsZ. ACS Chem. Biol. 12, 1947–1955 (2017).
Google Scholar
-
Rosado-Lugo, J. D. et al. Evaluation of 2,6-difluoro-3-(oxazol-2-ylmethoxy)benzamide chemotypes as Gram-negative FtsZ inhibitors. J. Antibiot. 75, 385–395 (2022).
Google Scholar
-
Andreu, J. M., Huecas, S., Araujo-Bazan, L., Vazquez-Villa, H. & Martin-Fontecha, M. The search for antibacterial inhibitors targeting cell division protein FtsZ at its nucleotide and allosteric binding sites. Biomedicines 10, 1825 (2022).
Google Scholar
-
Du, R. L. et al. Discovery of FtsZ inhibitors by virtual screening as antibacterial agents and study of the inhibition mechanism. RSC Med. Chem. 13, 79–89 (2022).
Google Scholar
-
Naz, F. et al. Screening of plant-based natural compounds as an inhibitor of FtsZ from Salmonella Typhi using the computational, biochemical and in vitro cell-based studies. Int. J. Biol. Macromol. 219, 428–437 (2022).
Google Scholar
-
Slade, J. A., Brockett, M., Singh, R., Liechti, G. W. & Maurelli, A. T. Fosmidomycin, an inhibitor of isoprenoid synthesis, induces persistence in Chlamydia by inhibiting peptidoglycan assembly. PLoS Pathog. 15, e1008078 (2019).
Google Scholar
-
Sanders, S. et al. Growth medium-dependent antimicrobial activity of early stage MEP pathway inhibitors. PLoS ONE 13, e0197638 (2018).
Google Scholar
-
Wang, X. & Dowd, C. S. The methylerythritol phosphate pathway: promising drug targets in the fight against tuberculosis. ACS Infect. Dis. 4, 278–290 (2018).
Google Scholar
-
Singh, K. S. et al. IspH inhibitors kill Gram-negative bacteria and mobilize immune clearance. Nature 589, 597–602 (2021).
Google Scholar
-
Allamand, A., Piechowiak, T., Lièvremont, D., Rohmer, M. & Grosdemange-Billiard, C. The multifaceted mep pathway: towards new therapeutic perspectives. Molecules 28, 1403 (2023).
Google Scholar
-
Knak, T. et al. Over 40 years of fosmidomycin drug research: a comprehensive review and future opportunities. Pharmaceuticals 15, 1553 (2022).
Google Scholar
-
Jobelius, H., Bianchino, G. I., Borel, F., Chaignon, P. & Seemann, M. The reductive dehydroxylation catalyzed by IspH, a source of inspiration for the development of novel anti-infectives. Molecules 27, 708 (2022).
Google Scholar
-
Zhang, Y. M., White, S. W. & Rock, C. O. Inhibiting bacterial fatty acid synthesis. J. Biol. Chem. 281, 17541–17544 (2006).
Google Scholar
-
Allahverdiyev, A. M. et al. The use of platensimycin and platencin to fight antibiotic resistance. Infect. Drug Resist. 6, 99 (2013).
Google Scholar
-
Bibens, L., Becker, J.-P., Dassonville-Klimpt, A. & Sonnet, P. A review of fatty acid biosynthesis enzyme inhibitors as promising antimicrobial drugs. Pharmaceuticals 16, 425 (2023).
Google Scholar
-
Parker, E. N. et al. An iterative approach guides discovery of the FabI inhibitor fabimycin, a late-stage antibiotic candidate with in vivo efficacy against drug-resistant Gram-negative infections. ACS Cent. Sci. 8, 1145–1158 (2022).
Google Scholar
-
Yao, J. & Rock, C. O. Resistance mechanisms and the future of bacterial Enoyl-Acyl carrier protein reductase (FabI) antibiotics. Cold Spring Harb. Perspect. Med. 6, a027045 (2016).
Google Scholar
-
Leonardi, R. & Jackowski, S. Biosynthesis of pantothenic acid and coenzyme A. EcoSal Plus 2, https://doi.org/10.1128/ecosalplus.3.6.3.4 (2007).
-
Chiarelli, L. R. et al. A multitarget approach to drug discovery inhibiting Mycobacterium tuberculosis PyrG and PanK. Sci. Rep. 8, 3187 (2018).
Google Scholar
-
Shapiro, J. A. et al. Identification of specific and nonspecific inhibitors of Bacillus anthracis type III pantothenate kinase (PanK). ChemMedChem 14, 78–82 (2019).
Google Scholar
-
Moolman, W. J., de Villiers, M. & Strauss, E. Recent advances in targeting coenzyme A biosynthesis and utilization for antimicrobial drug development. Biochem. Soc. Trans. 42, 1080–1086 (2014).
Google Scholar
-
Miller, J. R. et al. Phosphopantetheine adenylyltransferase from Escherichia coli: investigation of the kinetic mechanism and role in regulation of coenzyme A biosynthesis. J. Bacteriol. 189, 8196–8205 (2007).
Google Scholar
-
Gupta, A., Sharma, P., Singh, T. P. & Sharma, S. Phosphopantetheine adenylyltransferase: a promising drug target to combat antibiotic resistance. Biochim. Biophys. Acta 1869, 140566 (2021).
Google Scholar
-
de Jonge, B. L. et al. Discovery of inhibitors of 4′-phosphopantetheine adenylyltransferase (PPAT) to validate PPAT as a target for antibacterial therapy. Antimicrob. Agents Chemother. 57, 6005–6015 (2013).
Google Scholar
-
Sibon, O. C. & Strauss, E. Coenzyme A: to make it or uptake it? Nat. Rev. Mol. Cell Biol. 17, 605–606 (2016).
Google Scholar
-
Rath, C. M. et al. Optimization of CoaD inhibitors against Gram-negative organisms through targeted metabolomics. ACS Infect. Dis. 4, 391–402 (2018).
Google Scholar
-
Skepper, C. K. et al. Discovery and optimization of phosphopantetheine adenylyltransferase inhibitors with Gram-negative antibacterial activity. J. Med. Chem. 61, 3325–3349 (2018).
Google Scholar
-
Motika, S. E. et al. Gram-negative antibiotic active through inhibition of an essential riboswitch. J. Am. Chem. Soc. 142, 10856–10862 (2020).
Google Scholar
-
Howe, J. A. et al. Selective small-molecule inhibition of an RNA structural element. Nature 526, 672–677 (2015).
Google Scholar
-
Howe, J. A. et al. Atomic resolution mechanistic studies of ribocil: a highly selective unnatural ligand mimic of the E. coli FMN riboswitch. RNA Biol. 13, 946–954 (2016).
Google Scholar
-
Panchal, V. & Brenk, R. Riboswitches as drug targets for antibiotics. Antibiotics 10, 45 (2021).
Google Scholar
-
Wang, H. et al. Dual-targeting small-molecule inhibitors of the Staphylococcus aureus FMN riboswitch disrupt riboflavin homeostasis in an infectious setting. Cell Chem. Biol. 24, 576–588.e6 (2017).
Google Scholar
-
Sirithanakorn, C. & Cronan, J. E. Biotin, a universal and essential cofactor: synthesis, ligation and regulation. FEMS Microbiol. Rev. 45, fuab003 (2021).
Google Scholar
-
Park, S. W. et al. Target-based identification of whole-cell active inhibitors of biotin biosynthesis in Mycobacterium tuberculosis. Chem. Biol. 22, 76–86 (2015).
Google Scholar
-
Zlitni, S., Ferruccio, L. F. & Brown, E. D. Metabolic suppression identifies new antibacterial inhibitors under nutrient limitation. Nat. Chem. Biol. 9, 796–804 (2013).
Google Scholar
-
Carfrae, L. A. et al. Mimicking the human environment in mice reveals that inhibiting biotin biosynthesis is effective against antibiotic-resistant pathogens. Nat. Microbiol. 5, 93–101 (2020).
Google Scholar
-
Ma, C., Yang, X. & Lewis, P. J. Bacterial transcription as a target for antibacterial drug development. Microbiol. Mol. Biol. Rev. 80, 139–160 (2016).
Google Scholar
-
Mosaei, H. & Harbottle, J. Mechanisms of antibiotics inhibiting bacterial RNA polymerase. Biochem. Soc. Trans. 47, 339–350 (2019).
Google Scholar
-
Nogales, E., Louder, R. K. & He, Y. Structural insights into the eukaryotic transcription initiation machinery. Annu. Rev. Biophys. 46, 59–83 (2017).
Google Scholar
-
Babakhani, F., Seddon, J. & Sears, P. Comparative microbiological studies of transcription inhibitors fidaxomicin and the rifamycins in Clostridium difficile. Antimicrob. Agents Chemother. 58, 2934–2937 (2014).
Google Scholar
-
Vior, N. M. et al. Discovery and biosynthesis of the antibiotic bicyclomycin in distantly related bacterial classes. Appl. Environ. Microbiol. 84, e02828–17 (2018).
Google Scholar
-
Eidem, T. M., Roux, C. M. & Dunman, P. M. RNA decay: a novel therapeutic target in bacteria. Wiley Interdiscip. Rev. RNA 3, 443–454 (2012).
Google Scholar
-
Mackie, G. A. RNase E: at the interface of bacterial RNA processing and decay. Nat. Rev. Microbiol. 11, 45–57 (2013).
Google Scholar
-
Kime, L. et al. The first small-molecule inhibitors of members of the ribonuclease E family. Sci. Rep. 5, 8028 (2015).
Google Scholar
-
Mardle, C. E. et al. Identification and analysis of novel small molecule inhibitors of RNase E: implications for antibacterial targeting and regulation of RNase E. Biochem. Biophys. Rep. 23, 100773 (2020).
Google Scholar
-
Tsai, Y. C. et al. Recognition of the 70S ribosome and polysome by the RNA degradosome in Escherichia coli. Nucleic Acids Res. 40, 10417–10431 (2012).
Google Scholar
-
Prats-Ejarque, G. et al. Structure-based design of an RNase chimera for antimicrobial therapy. Int. J. Mol. Sci./ 23, 95 (2021).
Google Scholar
-
Chopra, S. & Reader, J. tRNAs as antibiotic targets. Int. J. Mol. Sci. 16, 321–349 (2014).
Google Scholar
-
de Crécy-Lagard, V. & Jaroch, M. Functions of bacterial tRNA modifications: from ubiquity to diversity. Trends Microbiol. 29, 41–53 (2021).
Google Scholar
-
Masuda, I. et al. tRNA methylation is a global determinant of bacterial multi-drug resistance. Cell Syst. 8, 302–314.e8 (2019).
Google Scholar
-
Zhong, W. et al. Thienopyrimidinone derivatives that inhibit bacterial tRNA (guanine37-N(1))-methyltransferase (TrmD) by restructuring the active site with a tyrosine-flipping mechanism. J. Med. Chem. 62, 7788–7805 (2019).
Google Scholar
-
Goto-Ito, S., Ito, T. & Yokoyama, S. Trm5 and TrmD: two enzymes from distinct origins catalyze the identical tRNA modification, m(1)G37. Biomolecules 7, 32 (2017).
Google Scholar
-
Jaroensuk, J. et al. Crystal structure and catalytic mechanism of the essential m1G37 tRNA methyltransferase TrmD from Pseudomonas aeruginosa. RNA 25, 1481–1496 (2019).
Google Scholar
-
Zhong, W. et al. Targeting the bacterial epitranscriptome for antibiotic development: discovery of novel tRNA-(N1G37) methyltransferase (TrmD) inhibitors. ACS Infect. Dis. 5, 326–335 (2019).
Google Scholar
-
Hill, P. J. et al. Selective inhibitors of bacterial t-RNA-(N1G37) methyltransferase (TrmD) that demonstrate novel ordering of the lid domain. J. Med. Chem. 56, 7278–7288 (2013).
Google Scholar
-
Pang, L., Weeks, S. D. & Van Aerschot, A. Aminoacyl-tRNA synthetases as valuable targets for antimicrobial drug discovery. Int. J. Mol. Sci. 22, 1750 (2021).
Google Scholar
-
Francklyn, C. S. & Mullen, P. Progress and challenges in aminoacyl-tRNA synthetase-based therapeutics. J. Biol. Chem. 294, 5365–5385 (2019).
Google Scholar
-
Cai, Z. et al. Design, synthesis, and proof-of-concept of triple-site inhibitors against aminoacyl-tRNA synthetases. J. Med. Chem. 65, 5800–5820 (2022).
Google Scholar
-
Harvey, K. L., Jarocki, V. M., Charles, I. G. & Djordjevic, S. P. The diverse functional roles of elongation factor Tu (EF-Tu) in microbial pathogenesis. Front. Microbiol. 10, 2351 (2019).
Google Scholar
-
Arenz, S. & Wilson, D. N. Bacterial protein synthesis as a target for antibiotic inhibition. Cold Spring Harb. Perspect. Med. 6, a025361 (2016).
Google Scholar
-
Masschelein, J. et al. A dual transacylation mechanism for polyketide synthase chain release in enacyloxin antibiotic biosynthesis. Nat. Chem. 11, 906–912 (2019).
Google Scholar
-
Fields, F. R., Lee, S. W. & McConnell, M. J. Using bacterial genomes and essential genes for the development of new antibiotics. Biochem. Pharmacol. 134, 74–86 (2017).
Google Scholar
-
Prajapati, J. D., Kleinekathöfer, U. & Winterhalter, M. How to enter a bacterium: bacterial porins and the permeation of antibiotics. Chem. Rev. 121, 5158–5192 (2021).
Google Scholar
-
Acosta-Gutiérrez, S. et al. Getting drugs into Gram-negative bacteria: rational rules for permeation through general porins. ACS Infect. Dis. 4, 1487–1498 (2018).
Google Scholar
-
Davis, T. D., Gerry, C. J. & Tan, D. S. General platform for systematic quantitative evaluation of small-molecule permeability in bacteria. ACS Chem. Biol. 9, 2535–2544 (2014).
Google Scholar
-
Richter, M. F. et al. Predictive compound accumulation rules yield a broad-spectrum antibiotic. Nature 545, 299–304 (2017).
Google Scholar
-
Farha, M. A. & Brown, E. D. Unconventional screening approaches for antibiotic discovery. Ann. NY Acad. Sci. 1354, 54–66 (2015).
Google Scholar
-
Dheman, N. et al. An analysis of antibacterial drug development trends in the united states, 1980–2019. Clin. Infect. Dis. 73, e4444–e4450 (2021).
Google Scholar
-
Drakeman, D. & Oraiopoulos, N. The risk of de-risking innovation: optimal R&D strategies in ambiguous environments. Calif. Manag. Rev. 62, 42–63 (2020).
Google Scholar
-
Theuretzbacher, U., Baraldi, E., Ciabuschi, F. & Callegari, S. Challenges and shortcomings of antibacterial discovery projects. Clin. Microbiol. Infect. 29, 610–615 (2023).
Google Scholar
-
Cook, M. A. & Wright, G. D. The past, present, and future of antibiotics. Sci. Transl Med. 14, eabo7793 (2022).
Google Scholar
-
Jones, L. H. An industry perspective on drug target validation. Expert Opin. Drug Discov. 11, 623–625 (2016).
Google Scholar
-
Zhu, F. et al. Update of TTD: therapeutic target database. Nucleic Acids Res. 38, D787–D791 (2010).
Google Scholar
-
Chen, L., Oughtred, R., Berman, H. M. & Westbrook, J. TargetDB: a target registration database for structural genomics projects. Bioinformatics 20, 2860–2862 (2004).
Google Scholar
-
Magarinos, M. P. et al. TDR targets: a chemogenomics resource for neglected diseases. Nucleic Acids Res. 40, D1118–D1127 (2012).
Google Scholar
-
Sosa, E. J. et al. Target-Pathogen: a structural bioinformatic approach to prioritize drug targets in pathogens. Nucleic Acids Res. 46, D413–D418 (2018).
Google Scholar
-
Le Guilloux, V., Schmidtke, P. & Tuffery, P. Fpocket: an open source platform for ligand pocket detection. BMC Bioinformatics 10, 168 (2009).
Google Scholar
Acknowledgements
The authors thank H.-K. Ropponen for help for searching target inhibitors in the literature, and L. Silver and L. Czaplewski for constructive feedback on content. Global Antibiotic Research and Development Partnership (GARDP) is currently funded by the governments of Australia, Germany, Japan, Monaco, The Netherlands, the Public Health Agency of Canada, South Africa, Switzerland, the United Kingdom, the Canton of Geneva, as well as the European Union, Wellcome Trust and private foundations.
Author information
Authors and Affiliations
Contributions
All authors contributed to the writing of this article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Drug Discovery thanks Todd Black and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Prokaryotics pipeline:
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and Permissions
About this article
Cite this article
Theuretzbacher, U., Blasco, B., Duffey, M. et al. Unrealized targets in the discovery of antibiotics for Gram-negative bacterial infections.
Nat Rev Drug Discov (2023). https://doi.org/10.1038/s41573-023-00791-6
-
Accepted: 15 August 2023
-
Published: 13 October 2023
-
DOI: https://doi.org/10.1038/s41573-023-00791-6