You’ll want to know to get the right treatment.
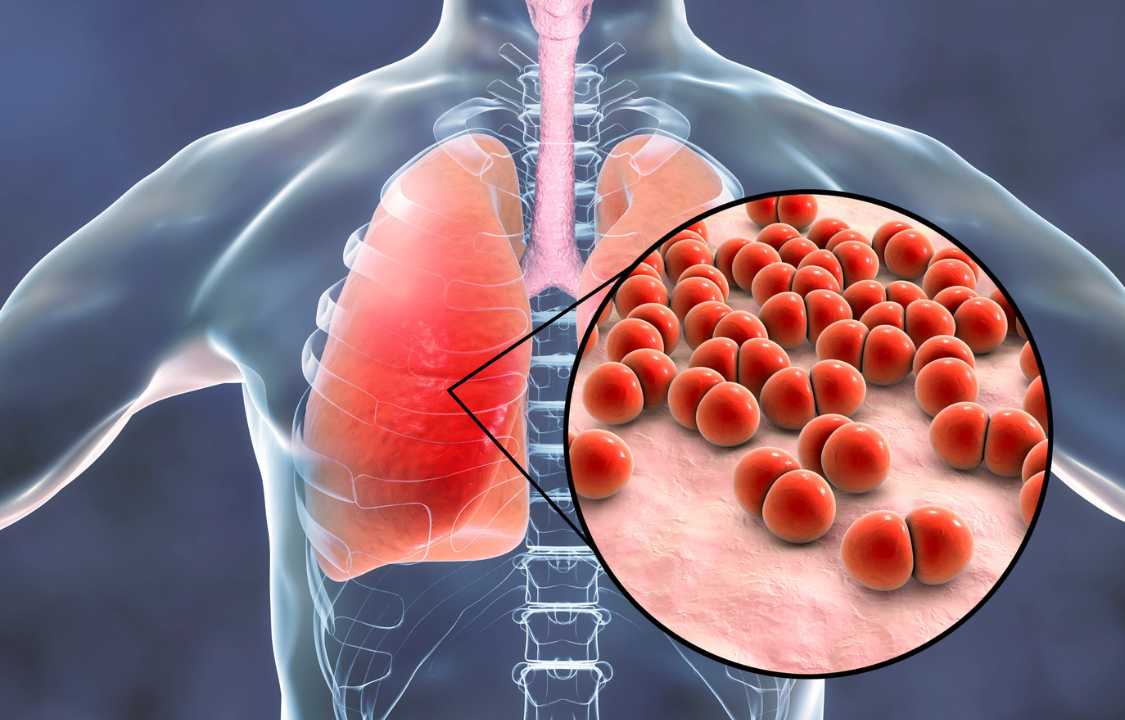
Pneumonia, a respiratory infection that affects the lungs, is a condition that can be caused by various agents, with viral and bacterial pneumonia being among the most common types. These two forms of pneumonia share some similarities but also have crucial differences in terms of treatment and severity. In this comprehensive exploration, we will delve into the causes, symptoms, prevention, and treatment of viral and bacterial pneumonia while also discussing other lesser-known variants of the disease.
Understanding the Causes
The root cause of pneumonia depends on its type. Viral pneumonia can be attributed to a wide range of viruses, including those responsible for common illnesses like the cold and influenza. Viral pneumonia is particularly contagious and can easily spread from person to person through close contact, making it a concern in shared spaces such as workplaces, households, and public transportation. Fortunately, most cases of viral pneumonia are mild, and patients typically experience improvement within a few weeks, according to the National Heart, Lung, and Blood Institute (NHLBI).
On the other hand, bacterial pneumonia often develops as a secondary infection following a preceding illness, such as the common cold or the flu. Unlike viral pneumonia, bacterial pneumonia is less contagious and does not typically spread from person to person. Streptococcus pneumoniae, a bacterium commonly found in the throats of many individuals without causing harm, is a leading cause of bacterial pneumonia. However, individuals with compromised immune systems or underlying health conditions are at a higher risk of developing pneumonia if their immune defenses are weakened.
Apart from viral and bacterial pneumonia, there exists a less common but noteworthy variant known as fungal pneumonia. This type primarily affects individuals with weakened immune systems due to specific medical conditions. Additionally, necrotizing pneumonia, a rare yet severe form of bacterial pneumonia, and cryptogenic organizing pneumonia, an uncommon disease with unknown causes treated with steroids, are other pneumonia variants worth noting. The term “walking pneumonia” is also familiar, describing a mild form of pneumonia where individuals may not realize they are ill and can continue their daily activities with relatively mild symptoms.
Prevention Measures
Preventing pneumonia, regardless of its type, hinges on good hygiene practices and maintaining overall health. Key prevention measures include:
1. Hand Hygiene: Regularly washing hands with soap and water is a fundamental step in preventing the transmission of infectious agents.
2. Avoiding Close Contact: Steer clear of individuals who are actively sneezing or coughing, as respiratory droplets are a common mode of transmission for pneumonia.
3. Surface Cleaning: Regularly disinfect frequently touched surfaces like elevator buttons, door handles, and doorknobs to reduce the persistence of germs.
4. Maintaining a Strong Immune System: Eating a balanced diet, staying hydrated, and ensuring adequate sleep can help bolster the body’s natural defenses.
Vaccination plays a crucial role in pneumonia prevention. Annual flu vaccines are recommended to reduce the risk of influenza, which can lead to pneumonia. Furthermore, the pneumococcal vaccine is advised for individuals aged 65 and older, as well as for smokers and younger people with specific medical conditions. This vaccine provides protection against bacterial pneumonia.
Similar Symptoms, Different Causes
Both viral and bacterial pneumonia share several common symptoms, including coughing with the production of sputum, fever, shortness of breath, and chest pain during coughing or deep breathing. These symptoms can make it challenging to differentiate between the two based solely on clinical presentation.
However, it is essential to note that bacterial pneumonia tends to cause more severe symptoms compared to its viral counterpart. The severity of symptoms often serves as a critical clue for healthcare providers when determining the type of pneumonia.
Treatment Approaches
Accurate diagnosis is pivotal in determining the appropriate treatment for pneumonia. Healthcare providers employ various diagnostic tools, such as sputum cultures, chest X-rays, and blood tests, to distinguish between viral and bacterial pneumonia.
If the diagnosis points to viral pneumonia, antibiotics are not the recommended course of action since antibiotics are ineffective against viruses. Instead, antiviral medications or over-the-counter drugs to alleviate symptoms are typically prescribed. For instance, Tylenol can be used to reduce fever, while expectorants help thin mucus, facilitating more productive coughing.
In cases of bacterial pneumonia, antibiotics are the primary mode of treatment. The choice of antibiotics may vary depending on the specific bacteria causing the infection, and healthcare providers may need to adjust the treatment based on the patient’s response.
In conclusion, pneumonia, a diverse and multifaceted respiratory ailment, indeed presents itself in various forms, each with its distinctive attributes and approaches to treatment. These divergent manifestations, including viral, bacterial, and other less common variants like fungal pneumonia, necrotizing pneumonia, and cryptogenic organizing pneumonia, underscore the complexity of this respiratory condition. It is imperative to recognize that while pneumonia can be a formidable illness, there exist effective strategies to mitigate its impact and expedite recovery.
Preventative measures, including vaccination against influenza and pneumococcal pneumonia, play a pivotal role in reducing the risk of contracting this ailment. Additionally, maintaining meticulous hygiene practices, such as frequent handwashing and respiratory etiquette, further bolsters the defense against pneumonia-causing pathogens. A nutritious diet, regular physical activity, and adequate sleep fortify the immune system, enhancing its ability to fend off respiratory infections.
Crucially, pneumonia demands a nuanced approach to diagnosis and treatment. Timely and precise identification of the specific type of pneumonia is vital for tailoring an effective treatment plan. Healthcare providers employ a spectrum of diagnostic tools, encompassing physical examinations, chest X-rays, blood tests, and sputum cultures, to differentiate between viral and bacterial pneumonia and other pneumonia variants. This tailored approach ensures that patients receive the most appropriate and effective interventions for their unique circumstances.
While pneumonia, particularly in its severe forms, poses a significant health risk, knowledge and preparedness are potent weapons in the battle against it. With a deep understanding of the disease’s varied presentations and a commitment to preventive measures, individuals can significantly reduce their vulnerability. Moreover, early detection and prompt treatment can transform pneumonia from a potentially life-threatening condition into a manageable and survivable one.
In this ever-evolving landscape of healthcare, ongoing research and innovation continue to expand our understanding of pneumonia and refine our strategies for its prevention and management. With the collaborative efforts of healthcare providers, researchers, and informed individuals, we are better equipped than ever to confront pneumonia and its multifaceted challenges. In doing so, we can ensure that pneumonia, while still a formidable adversary, need not be an insurmountable one.