Cardiovascular
Orthostatic Hypotension, Hypertension Treatment, and Cardiovascular Disease
Key Points
Question
Does the effect of intensive blood pressure treatment on cardiovascular disease or all-cause mortality differ based on the presence or absence of orthostatic or standing hypotension?
Findings
In this individual data meta-analysis of more than 29 000 participants in 9 hypertension trials, more intensive blood pressure treatment lowered risk of cardiovascular disease or all-cause mortality regardless of whether participants had orthostatic hypotension. Moreover, effects did not differ by the presence or absence of standing hypotension.
Meaning
Asymptomatic orthostatic hypotension or standing hypotension among adults with hypertension should not be a deterrent to more intensive hypertension treatment.
Importance
There are ongoing concerns about the benefits of intensive vs standard blood pressure (BP) treatment among adults with orthostatic hypotension or standing hypotension.
Objective
To determine the effect of a lower BP treatment goal or active therapy vs a standard BP treatment goal or placebo on cardiovascular disease (CVD) or all-cause mortality in strata of baseline orthostatic hypotension or baseline standing hypotension.
Data Sources
Individual participant data meta-analysis based on a systematic review of MEDLINE, EMBASE, and CENTRAL databases through May 13, 2022.
Study Selection
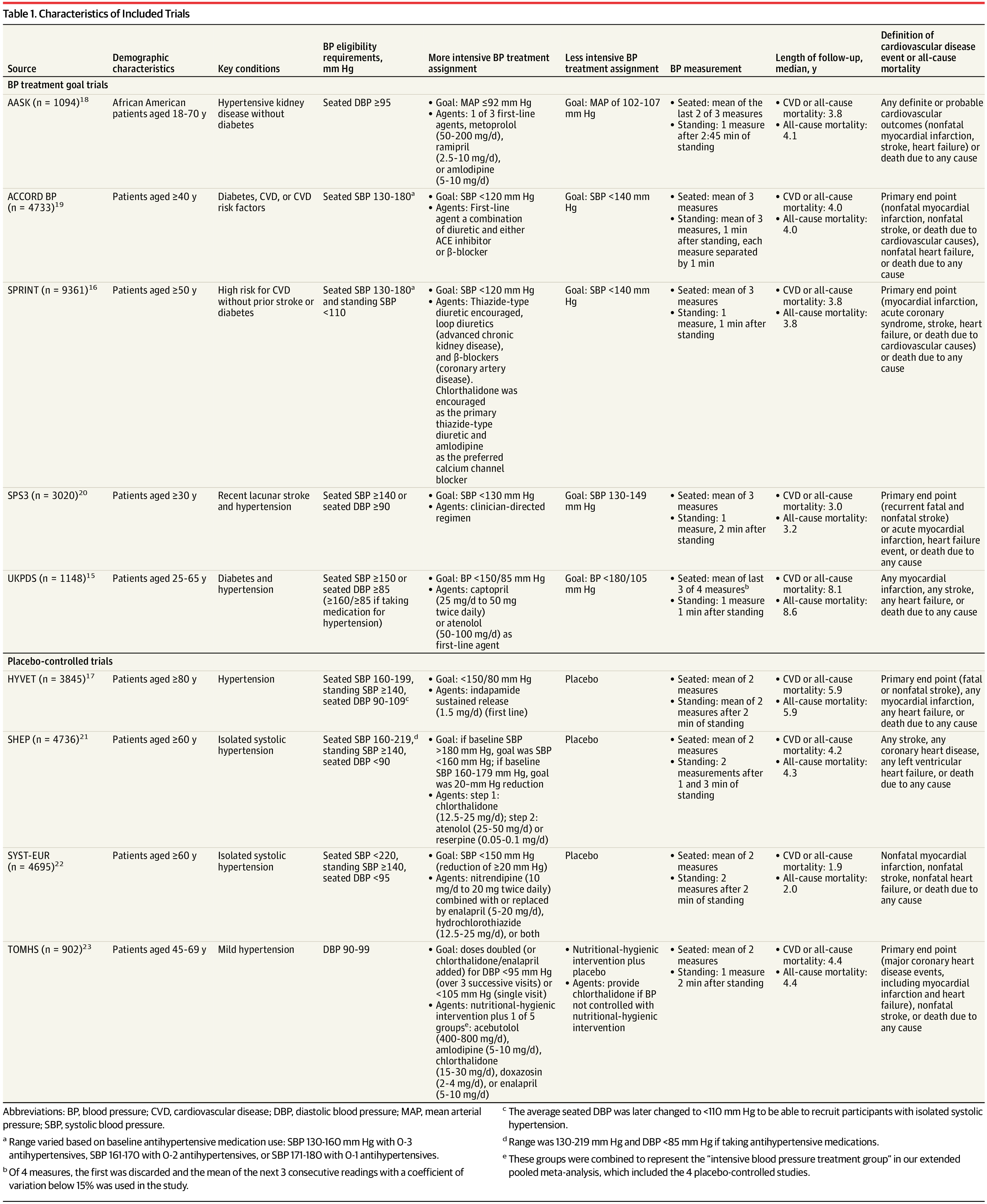
Randomized trials of BP pharmacologic treatment (more intensive BP goal or active agent) with orthostatic hypotension assessments.
Data Extraction and Synthesis
Individual participant data meta-analysis extracted following PRISMA guidelines. Effects were determined using Cox proportional hazard models using a single-stage approach.
Main Outcomes and Measures
Main outcomes were CVD or all-cause mortality. Orthostatic hypotension was defined as a decrease in systolic BP of at least 20 mm Hg and/or diastolic BP of at least 10 mm Hg after changing position from sitting to standing. Standing hypotension was defined as a standing systolic BP of 110 mm Hg or less or standing diastolic BP of 60 mm Hg or less.
Results
The 9 trials included 29 235 participants followed up for a median of 4 years (mean age, 69.0 [SD, 10.9] years; 48% women). There were 9% with orthostatic hypotension and 5% with standing hypotension at baseline. More intensive BP treatment or active therapy lowered risk of CVD or all-cause mortality among those without baseline orthostatic hypotension (hazard ratio [HR], 0.81; 95% CI, 0.76-0.86) similarly to those with baseline orthostatic hypotension (HR, 0.83; 95% CI, 0.70-1.00; P = .68 for interaction of treatment with baseline orthostatic hypotension). More intensive BP treatment or active therapy lowered risk of CVD or all-cause mortality among those without baseline standing hypotension (HR, 0.80; 95% CI, 0.75-0.85), and nonsignificantly among those with baseline standing hypotension (HR, 0.94; 95% CI, 0.75-1.18). Effects did not differ by baseline standing hypotension (P = .16 for interaction of treatment with baseline standing hypotension).
Conclusions and Relevance
In this population of hypertension trial participants, intensive therapy reduced risk of CVD or all-cause mortality regardless of orthostatic hypotension without evidence for different effects among those with standing hypotension.