Congenital disorders
Biliary sepsis complication with congenital hepatic fibrosis: an unexpected outcome
On July 8, 2022, a 23-year-old female patient presented with fever and diarrhea on admission. Physical examination revealed enlarged spleen 3 cm below the left costal margin. She denied any previous history of diseases. Her family history showed no consanguineous marriages.
Blood routine examination showed leukocytosis (WBC, white blood cell 18 × 10^9/L, ref: 3.50–9.50 × 10^9/L), thrombocytopenia (PLT, platelet, 39 × 10^9/L, ref:125–350 × 10^9/L), increased levels of ultrasensitive CRP (C-reactive protein, 288.5 mg/L, ref:<10 mg/L) and PCT (Pre-calcitoninogen, 42.6 ng/ml, ref: <0.5 ng/ml). Biochemical tests showed elevated levels of ALT ( alanine transaminase, 59 U/L, ref: 0–40 U/L), AST ( aspartate aminotransferase, 72 U/L, ref: 0–40 U/L), TBIL ( total bilirubin, 26 µmol/L, ref: 0–23 µmol/L), DBIL (direct bilirubin, 11.7µmol/L, ref: 0–4 µmol/L), TBA ( total bile acid, 119.1 µmol/L, ref: 0–10 µmol/L), SCr ( creatinine, 241 µmol/L, ref: 21–75 µmol/L), and decreased level of ALB ( albumin, 29 g/L, ref: 40–55 g/L). Serum liver fibrosis indicators showed elevated levels of HA ( hyaluronic acid, 502 ng/ml, ref: <100 ng/mL), PCIII ( Type III collagen, 33.2 ng/ml, ref: <30 ng/ml), and IV-C (Collagen type IV, 41. 2 ng/ml, ref: 1200 U/ml, ref: <39 U/ml) and CA125 (Carbohydrate antigen 125, 80.8 U/ml, ref: <39 U/ml). Serologic tests for viral hepatitis, autoantibodies, and platelet antibodies were negative. Serum IgM (Immunoglobulin M) and IgG (Immunoglobulin G) levels were normal. Serum ceruloplasmin levels and 24-hour urinary copper levels were normal, and ophthalmological examination revealed no evidence of the KF ring ( Kayser-Fleischer Ring ). Serum-ferritin, serum-iron and serum-total iron binding capacity were also all within normal ranges. Common liver diseases mainly include viral hepatitis, autoimmune hepatitis, drug-induced liver damage, metabolic liver disease including Wilson’s disease and hemochromatosis were excluded. Blood culture was positive for KP, and stool culture was positive for Candida albicans.
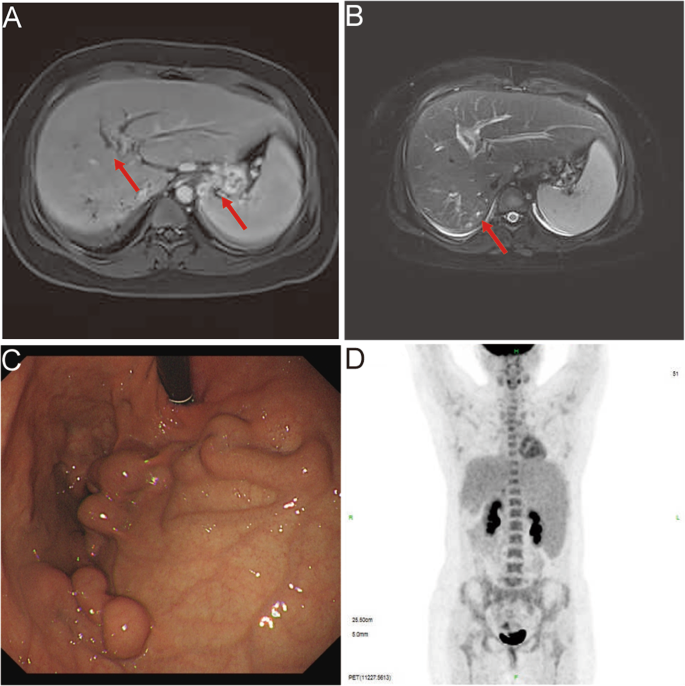
Further, CT (Computed tomography) imaging revealed slight striate shadow in the lower lobes of both lungs, a slight enlargement of the liver’s left lobe, mild dilation of the intrahepatic bile ducts, splenomegaly, esophageal and gastric fundus varices, and numerous tiny cysts in both kidneys. MRI (magnetic resonance imaging) revealed dilated intrahepatic and common bile ducts (Fig. 1 A-B). Upper gastrointestinal endoscopy revealed gastric fundus varices without red signs (Fig. 1 C). Since the patient had elevated serum tumor markers (CA19-9 level>1200 U/ml, ref: <39 U/ml) and CA125 (80.8 U/ml, ref: <39 U/ml), with abnormal levels of ALT and AST, so PET/CT (positron emission tomography/computed tomography) was performed to exclude tumors. PET/CT findings suggested slightly enlarged liver with mild dilatation of the intrahepatic bile ducts, hyperplastic lymph nodes around the portal vein, giant spleen with no increase in FDG (fluorodeoxyglucose) metabolism (Fig. 1 D).
Imaging findings of the patient. (A-B) MRI imaging revealed dilated intrahepatic bile duct dilatation, gastric fundic varices, an enlarged spleen and small cyst in the kidney (arrow). (C) Upper gastrointestinal endoscopy revealed gastric fundic varices. (D) PET/CT imaging revealed slightly enlarged liver, hyperplastic lymph nodes around the portal vein, giant spleen with no increase in FDG metabolism and multiple varices in the fundic and retroperitoneum
Anti-bacterial therapy (Meropenem injection), anti-inflammatory therapy (Methylprednisolone Sodium Succinate injection), anti-diarrheal therapy (Montmorillonite powder and Loperamide Hydrochloride capsules), and platelet production-promoting therapy (Recombinant Human Thrombopoietin injection) were given. The patient was treated with for Loperamide for 1 day, anti- diarrheal therapy was stopped when symptom improved. After nearly one month of treatment, the levels of WBC, CRP, PCT, CA19-9/125, and liver fibrosis indexes returned to normal, and platelet count increased to 64 × 10^9/L. Biochemical tests revealed normal levels of ALT (16 U/L), AST (19 U/L), TBIL (12.4 µmol/L), DBIL (2.6 µmol/L), TBA (3.4 µmol/L), AKP (40 U/L), and SCr (72 µmol/L). Images revealed dilated intrahepatic bile ducts, full left lobe of liver, full gallbladder, enlarged spleen, and multiple varices in the esophagogastric fundus (Fig. 2 A-C).

Imaging findings at discharge and follow-up results of the patient. (A) MRI imaging revealed intrahepatic bile duct dilatation and gastric fundic varices (arrow). (B) MRI imaging revealed cystic dilatation of the intrahepatic bile duct (arrow). (C) MRCP imaging showed the morphological characteristics of bile duct tree
The patient underwent liver biopsies after receiving anti-infective therapy. The pathological findings of the liver biopsy showed several portal tracts are interconnected by bridging fibrous septa, which contained intensive proliferation of the bile ducts without inflammatory cell infiltrates, some of the bile ducts contained bile plugs (Fig. 3 A-C). Immunohistochemical CK7 (Cytokeratin 7), CK8/18 (Cytokeratin 8/18), and CK19 (Cytokeratin 19) staining in the liver tissue showed massive hyperplasia of irregular bile ducts and cystic dilatation of bile ducts (Fig. 2 D-F).

Liver biopsy of the patient. (A-B) H&E staining showed several portal tracts are interconnected by bridging fibrous septa, which contained intensive proliferation of the bile ducts, some of the bile ducts contained bile plugs (C) Masson staining revealed extensive formation of collagen fibers. (D-F) Immunohistochemistry CK7, CK8/18, and CK19 staining revealed a large amount of irregular bile duct, and bile duct cystic dilatation
Furthermore, whole-exome sequencing was performed, and compound heterozygous variants were identified in the PKHD1 gene (reference sequence NM_138694): two missense substitutions c.3860T > G (p. V1287G) and c.9059T > C (p. L3020P) (Fig. 4A). Both of the targeted variations were confirmed by Sanger sequencing in the index patient and her parents, c.3860T > G variant was paternally inherited, and c.9059T > C variant was maternally inherited (Fig. 4B). The in-silico analysis predicted the c. 3860T > G/p. V1287G variant as unknown clinical significance (SIFT score 0.029, damaging; Polyphen2 score 0.001, benign; REVEL score 0.226, tolerable; ClinPred score 0.02426, benign), and the c. 9059T > C/p. L3020P variant as deleterious (SIFT score 0.012, damaging; Polyphen2 score 0.984, probably damaging; REVEL score 0.841, damaging; ClinPred score 0.7198, pathogenic). Swiss Model homology modeling was performed to visualize three-dimensional structures with the two variations in the PKHD1 protein (Fig. 3C-D).

Analysis of gene mutation. (A) Whole-exome sequencing identified two heterozygous missense variants in the patient. (B) Sanger sequencing of the two targeted PKHD1 variations in the patient and her parents. The arrows indicate two heterozygous missense variants c.3860T > G and c.9059T > C. The arrows indicate her father carried c.3860T > G variant and were the wild-type genotype of c.9059T > C variant, her mother carried c.9059T > C variant and were the wild-type genotype of c.3860T > G variant. (C-D) Using PyMol to predicted the structure of PKHD1 with the variant PKHD1 of V1287G and p. L3020P, respectively. The difference in the side chains were indicated in yellow
A diagnosis of CHF complicated with biliary sepsis was made based on the patient’s laboratory tests, imaging findings, pathological and genetic results. No morphological changes in the liver were observed comparing liver imaging during and after biliary sepsis. After being discharged from the hospital, she took a small dose of carvedilol (10 mg once daily), a vasodilating beta-blocker, used to reduce the portal venous pressure. After nearly three months of portal hypotensive treatment, she had no symptoms such as fever, abdominal pain, vomiting of blood, black stools, and bloody stools. The levels of inflammatory markers were normal, serum detections of liver and kidney function were normal, while platelet counts declined to 44 × 10^9/L.