Infection
Respiratory Co-infections in COVID-19 Patients
Introduction
Since the first report of severe and critical acute respiratory syndrome coronavirus-2 (SARS-Cov-2) in December of 2019 in Wuhan, Hubei, China, it has rapidly spread to all regions of the world.1 As of now, there have been over 7.66 billion confirmed SARS-CoV-2 infections and at least 6.93 million reported deaths. (Last update: 16 May 2023, https://www.who.int/emergencies/diseases/novel-coronavirus-2019). The World Health Organization (WHO) declared the end of COVID-19’s emergency phase on May 5, 2023. However, due to insufficient vaccination rates, immune escape caused by mutations of SARS-CoV-2, and the imbalance of medical resources in different regions, the coronavirus disease 2019 (COVID-19) is expected to remain a significant threat to human health for an extended period in the future.2
Preceding viral infections, such as influenza and COVID-19, can impair antibacterial immunity, providing an opportunity for other colonizing pathogens, such as Streptococcus pneumoniae, Klebsiella pneumonia, to cause life-threatening second bacterial/viral pneumonias.3 The proportions of co-infections varies across studies, regions and populations, but it can exceed 50% deceased COVID-19 patients.4 This highlights the significance of co-infections as a crucial prognostic factor among these patients. The most frequently identified bacteria co-infections in COVID-19 patients include Klebsiella pneumoniae, Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae.5,6 The most common co-infecting viruses are influenza A virus (FluA), influenza B virus (FluB), respiratory syncytial virus (RSV) and coronavirus.5,6
Antibiotics are considered the most effective means of treating bacterial infections. However, there are concerns that the current epidemic has increased the risk of antibiotic abuse, potentially leading to an increased risk of drug-resistant bacterial infections.7 Although some reports on bacterial and viral co-infection exist,6,8 further investigation and research are still necessary and urgently needed in China, where the epidemic peak occurred after the adjustment of epidemic prevention policies in December, 2022. Understanding the occurrence of co-infection, evaluating the rationality of antibiotic use, and analyzing risk indications and risk factors in COVID-19 treatment are of paramount significance for the scientific management of COVID-19 in the future.
This study conducted a retrospective analysis of the clinical features of 716 COVID-19 inpatients in Guangxi province, China, during December 2022 to January 2023. Throat swabs were used for detecting the presence of 12 respiratory pathogens, which are most common and clinically significant in local hospital, through quantitative real-time polymerase chain reaction PCR (qPCR). Additionally, the study analyzed risk indicators that significantly influenced patient prognosis.
Materials and Methods
Clinical Data Collection
This study was conducted at the Affiliated Hospital of Youjiang Medical University for Nationalities in Guangxi, China, which is one of the important medical institutions in Southwest China. From December142022to January 30 2023, the COVID-19 patients admitted with COVID-19 were included in this study. The diagnosis and classification of COVID-19 followed the guidelines of the Diagnosis and treatment plan for SARS-Cov2 infection (10th Edition).9 Patient information, clinical manifestations, laboratory data, and treatment details were collected. All procedures involving human materials and electronic medical information were approved by the Medical Ethics Committee of Affiliated Hospital of Youjiang Medical University for Nationalities (Approval number: YYFY-LL-2023-119). Because all clinical data of hospitalized COVID-19 patients data used were fully anonymized, and no personal identifiers were accessible to the research team, the requirement for consent was waived.
Sample Collection and Respiratory Pathogen Detection
Throat swabs were collected from patients upon admission. SARS-Cov-2 was detected using the Detection Kit for 2019 Novel Coronavirus (2019-nCoV) RNA (PCR-Fluorescence Probing) (DaAnGene, DA0933) as per the manufacturer’s instructions. The 12 common pathogens causing respiratory tract infections were detected using the Six Respiratory Pathogens Multiplex Nucleic Acid Diagnostic Kit (Sansure, S3310E) and Six Respiratory Pathogens Nucleic Acid Diagnostic Kit (Sansure, S3066E) through qPCR analysis. The 12 detected pathogens include six bacteria (Klebsiella pneumoniae, Legionella pneumophila, Streptococcus pneumoniae, Haemophilus influenzae type b (Hib), Pseudomonas aeruginosa, Staphylococcus aureus), five viruses (Influenza A virus (FluA), Influenza B virus (FluB), Respiratory Syncytial Virus (RSV), Adenovirus (AdV), Human rhinovirus (HRV)), and Mycoplasma pneumoniae (Mp).
Statistical Analysis
The categorical variables were shown as numbers (percentages) and the continuous variables were shown as medians (interquartile ranges [IQRs]). Wilcoxon rank-sum test, Pearson’s Chi-squared test, and Fisher’s exact test were used to compare the distribution of categorical and continuous variables between the cohorts where appropriate. Chi square test was used to evaluate the correlation between categorical variables and Cramer’s V coefficient was used to assess the strength of association. The visualization of intersecting co-infection pathogens was performed by UpSetR (v1.4.0).10 The package StepReg (v1.4.4) and survival (v3.5.0) was used to perform univariable and multivariable Cox regression analysis. Forward steps method was used to select the major risk factors. All statistical analysis was conducted using R (v4.2.1).
Antiviral Treatments and Clinical Outcomes
Our hospital’s antiviral treatment and clinical outcomes for COVID-19 patients is primarily based on the “Diagnosis and treatment plan for SARS-Cov2 infection (10th Edition).9” Patients are categorized based on the severity of clinical symptoms. General treatment includes addressing the patient’s energy and nutritional intake, maintaining water and electrolyte balance, and managing fever and phlegm. Antiviral treatment is mainly administered based on the patient’s condition and may include medications such as Nirmatrelvir/Ritonavir tablets, Remdesivir tablets, monoclonal antibodies, and others. For severe and critical patients, timely organ function support is provided. Patients are categorized based on clinical indicators into four groups: mild, moderate, severe, and critical. Mild cases primarily exhibit upper respiratory tract infections. Patients with a continuous high fever for three days along with cough and shortness of breath, but a respiratory rate of 93%, are diagnosed as moderate. When the respiratory rate exceeds 30 breaths per minute, oxygen saturation falls below 93%, and there is progressive exacerbation of pulmonary lesions, the diagnosis is severe. Critical cases are diagnosed when respiratory failure, shock, or other organ dysfunction occurs. Patients can be considered for discharge when their vital signs stabilize, and there is a significant improvement in pulmonary lesions, allowing for a transition to oral medication treatment.
Results
Characteristics of COVID-19 Patients
As shown in Table 1, this study included a total of 716 COVID-19 patients who were hospitalized at Youjiang Affiliated Hospital for Nationalities during the period between December 14, 2022, and January 30, 2023. The selection of patients for the study was based on the diagnostic criteria outlined in the Diagnosis and Treatment Plan for SARS-Cov2 Infection (10th Edition).9 The data collected for analysis encompassed basic background information, information on any complications experienced by the patients, the medical interventions they received, and their clinical features at baseline. Among the 711 patients, a total of 440 (61%) were male, and the median age was 64 years old, with an interquartile range (IQR) of 49 to 73 years. Remarkably, a substantial majority of the patients, precisely 661 (92%) of them, had been vaccinated. Based on clinical typing, it was observed that 611 (65%) of the patients had moderate infections, 78 (11%) had severe infections, and 27 (3.8%) had critical infections. Over the course of the study, a total of 45 patients (6.3%) unfortunately died. In terms of hospital stay, the median length of hospitalization (LOHS) for the patients was 7 days, with an interquartile range (IQR) of 5 to 9 days. An investigation into the comorbidities exhibited by the patients revealed that the most common conditions were hypertension, affecting 184 patients (26%), and hypoproteinemia, affecting 172 patients (24%). Furthermore, an analysis of the predominant clinical signs among the patients indicated that the most common symptoms reported were cough, experienced by 524 patients (73%), and fever, reported by 217 patients (30%). In addition, we conducted a detailed analysis of the immunological characteristics among hospitalized COVID-19 patients with different disease severity grades (Table S1). The results showed that clinically key inflammatory markers, such as C-reactivate protein and D-dimer, showed a significant increase in severe and critical patients.
|
Table 1 Characteristics of Hospitalized COVID-19 Patients Included in This Study |
Co-Infection with Respiratory Pathogens in COVID-19 Patients
To investigate the co-infections in COVID-19 patients, we employed multiple fluorescence quantitative PCR to detect the presence of 12 crucial respiratory pathogens. The findings revealed that a substantial proportion of patients, up to 77% (550 out of 716), were affected by co-infections. Notably, we observed significant differences in the length of hospital stay and leukocyte counts between COVID-19 patients with co-infection and those without co-infection (refer to Table 1 for details). A detailed breakdown of the co-infection types showed that 529 patients (74%) had bacterial co-infections, while 108 patients (15%) had viral co-infections. Additionally, we identified 4 patients who were co-infected with Mp. Remarkably, about 12% of the patients exhibited concurrent co-infection with both bacteria and viruses. Surprisingly, there were no significant differences observed in the distribution of co-infection combinations among moderate, severe and critical cohorts (refer to Table 2).
 |
Table 2 Single and Multiple Co-Infections in Patients with SARS-CoV-2 Identified by the qPCR (n = 716) |
In the study, we identified a total of 12 respiratory pathogens, comprising 6 bacteria, 5 viruses, and 1 Mycoplasma (refer to Figure 1). Among these pathogens, all except Legionella pneumophila were detected in the patient cohort. The co-infecting pathogens detected in this study were as follows: S. pneumoniae (444, 62.01%), Hib (143, 19.97%), K. pneumoniae (82, 11.45%), P. aeruginosa (73, 10.20%), FluA (42, 5.87%), RSV (40, 5.59%), Adenovirus (27, 3.77%), S. aureus (26, 3.63%), FluB (13, 1.82%), Mp (4, 0.56%), and HRV (1, 0.14%) (see Figure S1). Of the cases analyzed, 304 (42.46%) showed detection of only one co-infected pathogen, with S. pneumoniae being the most common pathogen in such cases (220, 30.73%) (see Table S2). Regarding double pathogen detection, the most common combinations were S. pneumoniae – Hib (59, 8.24%), S. pneumoniae – FluA (25, 3.49%), and S. pneumoniae – K. pneumoniae (22, 3.07%). Furthermore, we observed that three-pathogen detection was also present, with the most common combinations being S. pneumoniae – Hib – K. pneumoniae (19, 2.65%) and S. pneumoniae – Hib – P. aeruginosa (9, 1.26%). Of particular interest was the detection of eight pathogens, namely S. pneumoniae, Hib, FluA, Adenovirus, S. aureus, FluB, Mp, and HRV, all in a single case.
|
Figure 1 The distribution of detected co-infection pathogens of cases in this study. The 12 pathogens were shown as rows of a matrix at the bottom, with intersections of pathogens indicated by connected filled circles, and the number of corresponding pathogens’ combinations shown as a bar plot above. |
Co-Infection with Patient Age and Disease Severity
Age has a notable impact on human immunity status. In this study, all twelve respiratory pathogens were detected in the 0–1 year age group, while eleven of them, except M. pneumoniae, were detected in individuals aged ≥65 years. Notably, the positive rate of S. pneumoniae was close to 50% (11/23) in cases aged 1–12 years old, significantly higher than in other age groups. Moreover, the positive rates of S. aureus and FluA in cases under 18 years old were significantly higher than in older age groups (refer to Table S3). In Table 3, we present the detection of several pathogens in the different disease categories, including moderate, severe, and critical cases. However, FluB, Mp, and HRV were exclusively detected in moderate disease cases. Interestingly, the detection rates of S. pneumoniae, RSV, and P. aeruginosa were significantly higher in moderate, severe, and critical disease cases, respectively, indicating potential associations between these pathogens and disease severity.
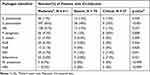 |
Table 3 Respiratory Pathogens Identified by the qPCR Among the Patients Tested in Different Disease Severity (n = 716) |
The analysis of antibiotic usage revealed that 65.5% (469 out of 716) of COVID-19 patients received antibiotic treatment in this cohort. Among the 550 cases that detected respiratory pathogens, 64.9% (357) of them received antibiotic treatment. And β-lactam antibiotics, cephalosporins, and quinolone antibiotics were the most widely used (refer to Figure S2). Surprisingly, even among cases with only virus co-infection (11 out of 21 cases) and cases without detection of any other respiratory pathogens (112 out of 166 cases), antibiotic treatment was administered to 52.4% and 67.5% of them, respectively (refer to Table S4). It is important to note that some patients might have received antibiotics for infections in other parts of the body (data not collected in this study). However, for most patients, the use of antibiotics might have been intended to prevent bacterial co-infections. This suggests that the use of antibiotics in primary hospitals may have exhibited a certain degree of irrationality.
Risk Factors Analyses of SARS-Cov2 Infection
Out of the 670 cases included in the risk factor analysis, 44 cases resulted in mortality, while 46 cases were excluded due to missing data. All the collectable clinical factors were included in the Cox’s proportional hazards regression analysis, and forward steps method was used to select the major risk factors. The survival curve indicated significant survival differences between corresponding factor strata for dyspnea (p < 0.001), hypoproteinemia (p < 0.01), lymphocytes (p < 0.01), and the presence of M. pneumoniae infection (p < 0.001) (refer to Figure 2).
|
Figure 2 The outcome of COVID-19 patients under different risk factors. The Kaplan-Meier method and the Log rank test were used to compare the estimated survival according to different risk factors. Survival curves according to dyspnea (A), hypoproteinemia (B), lymphocytes (C) and the infection of M. pneumonia (D), separately. |
Univariable and multivariable Cox regression analyses were employed to identify potential risk factors. The results of the univariable Cox regression analysis demonstrated significant associations between dyspnea, hypoproteinemia, lymphocyte count, and the presence of M. pneumoniae infection with COVID-19 case mortality (refer to Table 4). Upon adjusting for other factors, cases with dyspnea exhibited a higher risk of death compared to cases without dyspnea (adjusted HR: 2.09, 95% CI: 1.11–3.95). Similarly, individuals with hypoproteinemia had an increased risk of death, with an adjusted HR of 1.95 (95% CI: 1.03–3.66). The lymphocyte count significantly correlated with the risk of death in COVID-19 patients. Those with lymphocyte counts lower than 0.8×109 cells/L faced an increased risk of death (adjusted HR [95% CI]: 1.99 [1.06–3.75]). However, individuals with lymphocyte counts greater than 4×109 cells/L did not exhibit a significant difference in the risk of death compared to those within the normal lymphocyte count range. Remarkably, co-infection with M. pneumoniae was associated with a substantially higher risk of death compared to cases without this co-infection (adjusted HR [95% CI]: 26.03 [3.29–206.06]).
|
Table 4 Factors Associated with the Death of Hospitalized COVID-19 Patients (n=670) |
Chi-square test was employed to analysis whether the dyspnea, low lymphopenia and hypoproteinemia are associated with the bacterial co-infections (refer to Table 5). The results showed that lymphopenia is associated with the co-infection of H. influenza, and hypoproteinemia is associated with the S. pneumonia, H. influenza, P. aeruginosa. This result indicates a significant correlation between the co-infection of these bacteria and two key clinical indicators, namely hypoproteinemia and lymphopenia, closely associated with COVID-19 outcomes. Furthermore, our study showed that antibiotics usage is associated with the hypoproteinemia and lymphopenia. This suggests that the use of antibiotics may be of significant importance in improving clinical symptoms in patients with bacterial co-infections. In addition, the results indicate a significant correlation between C-reactive protein and co-infections with S. pneumoniae and P. aeruginosa. Finally, in line with Cox regression analysis results, no significant association was observed between antibiotic use and the risk of death.
 |
Table 5 Correlation Between Dyspnea, Lymphopenia, Hypoproteinemia, C-Reactive Protein, Death and Co-Infection Bacteria |
Discussion
Over the past three years, China has implemented stringent, rapid, and coordinated control measures to curb the spread of SARS-CoV-2. These measures have proven effective in controlling COVID-19 outbreaks and safeguarding public health. As the epidemic situation evolves and with the increased vaccination coverage and accumulated experience in prevention and control, China has gradually relaxed its strict epidemic control strategy.11 However, these policy changes have resulted in a peak of COVID-19 infections,12 signaling the need for continuous vigilance. Co-infection is a significant factor influencing the poor prognosis of COVID-19 patients.13,14 Despite several studies exploring co-infections with SARS-CoV-2,5,6 there remains a dearth of research focusing on China’s primary hospitals after the adjustment of COVID-19 prevention and control policies. Such research can provide valuable insights to guide effective management strategies and improve patient care in the face of changing epidemic dynamics.
In this study, we conducted the detection of 12 important respiratory pathogens in hospitalized COVID-19 patients. The results revealed that more than 77% (550 out of 716) of the cases had co-infections with at least one pathogen. This finding indicates a notably higher co-infection rate in this cohort compared to the majority of previous reports. For instance, a meta-analysis of 118 studies reported a pooled prevalence of co-infection as 19% (95% CI: 14%-25%).4 Sreenath et al reported a co-infection rate of 46.5% in COVID-19 patients in India, with 13 pathogens detected.5 Several reasons contribute to the high rate of co-infection observed in our study. First, the cases included in this study were moderate or severe, and such patients tend to have a relatively higher co-infection rate.4 Second, the use of a high sensitivity qPCR detection method for broad-spectrum respiratory pathogens increased the positive detection rate compared to culture or PCR targeting limited strains. Third, the high density of patients in the hospital during the peak of the epidemic might have increased inter-personal transmission. It is important to note that a Chinese cohort study reported an even higher co-infection rate of 94.2% (242 out of 257 cases), with the detection of 39 species.6 These significant differences between various studies could be attributed to the characteristics of the cohort, the spectrum of species detected, the regional health level, and other relevant factors.
Bacterial co-infection has been identified as a significant influencing factor leading to poor prognosis in patients with viral pneumonia.15 Consistent with some previous studies,6,16 we observed that S. pneumonia, Hib and K. pneumonia were the most common co-infecting bacterial pathogens that detected in this COVID-19 cohort. These three bacterial species are commonly considered as oral and upper respiratory colonizers, which may elevate the risk of lower respiratory tract infections, particularly in patients with compromised immunity. Notably, S. pneumoniae was found to be more prevalent in COVID-19 cases than in healthy controls.17 Its colonization has been associated with alterations in immune responses and an increased risk of virus acquisition.18 Hib is known to cause pneumonia or acute meningitis, particularly in infants or children under the age of five.19 Furthermore, it has been reported that co-infection with hypervirulent K. pneumoniae can lead to fatal sepsis in COVID-19 patients.20 We observed multiple co-infections with various combinations of pathogens in our study, such as S. pneumoniae – Hib (59, 8.24%), S. pneumoniae – K. pneumoniae (22, 3.07%), S. pneumoniae – Hib – K. pneumoniae (19, 2.65%), and S. pneumoniae – Hib – P. aeruginosa (9, 1.26%), among others. The elevation of C-reactive protein and D-dimer, prominent inflammatory markers, was notably higher in severe and critical COVID-19 patients (refer to Table S1). Our findings underscore a significant correlation between CRP and co-infections involving S. pneumoniae and P. aeruginosa, aligning with prior research (refer to Table 5). Elevated levels of these markers are closely associated with bacterial co-infections in COVID-19, particularly with Streptococci, and pose a significant risk for severe cardiac complications, notably myocarditis.21 The hypervirulence and multi-antibiotic resistance of these co-infected bacteria pose challenges in the treatment of COVID-19. Multiple studies suggest that vaccination, particularly with pneumococcal and Hib vaccines, provides protection against symptomatic SARS-CoV-2 infection and reduces the risk of mortality.22–24 Based on these findings, it is recommended that a multivalent pneumonia vaccine be considered as a preventive measure to protect against pneumonia caused by the common co-infected bacteria during the COVID-19 pandemic.
SARS-CoV-2 co-infection with another virus, such as influenza and RSV, has been significantly associated with an increased risk of death compared to SARS-CoV-2 monoinfection.25 In this study, virus co-infection was detected in 15% of COVID-19 cases. It is reported that the implementation of COVID-19 prevention and control measures can concurrently lower the infection rate of other pathogens like influenza.26 Our study indicated that the most prevalent co-infection viruses were FluA (42, 5.87%), RSV (40, 5.59%), Adenovirus (27, 3.77%), and FluB (13, 1.82%). Complex interactions between different viral infections have been reported in the literature. For instance, Lei Bai et al found that co-infection with influenza A (FluA) enhanced SARS-CoV-2 infection,27 while another study showed that FluA and RSV could inhibit the replication of SARS-CoV-2.28 Further research is needed to reveal the specific nature of these interactions. However, the significant risk posed by multiple viral infections cannot be ignored. Influenza vaccinations significantly reduce risk of hospitalization and death,29,30 and vaccination remains the best means of preventing multi-viral infections, particularly among high-risk groups.31
The misuse and overuse of antibiotics have long been recognized as significant public health concerns, especially in the post-COVID-19 era.7 On one side, such practices are major contributors to the emergence of antibiotic resistance, which can complicate the treatment of co-infections in COVID-19 patients. On the other side, the use of antibiotics can disrupt the balance of the intestinal microecology. The dysbiosis of gut microflora has been linked to disease severity and impaired immune response in COVID-19 patients.32 In this COVID-19 cohort, 65.5% of patients received antibiotic treatment. However, the use of antibiotics did not always align with the detection of co-infected bacterial pathogens (Table S4). In clinical practice, some patients use antibiotics as a preventive treatment measure for co-infection events, which may also have a positive impact on prognosis for COVID-19 patients. However, more accurate and efficient detection methods may help us use antibiotics more rationally, thereby minimizing their potential negative effects. Therefore, to facilitate a more judicious use of antibiotics, it is advisable to expand the utilization of PCR and other clinical diagnostic tests for key infections, including S. pneumoniae, Haemophilus, Klebsiella, and Pseudomonas. This strategic approach ensures that antibiotic treatment is reserved for patients with genuine clinical indications, thereby minimizing unnecessary antibiotic exposure.
Risk factor analysis was conducted to investigate the relationship between death and clinical features in COVID-19 cases. Dyspnea, a crucial clinical feature of lower respiratory tract infection and pneumonia, emerged as a significant risk factor for death based on the results of univariable and multivariable Cox regression analysis. This finding highlights the importance of prompt hospital admission for patients experiencing breathing difficulties to ensure timely and professional treatment. Furthermore, the analysis revealed that hypoproteinemia was a significant risk factor for death in COVID-19 patients. Hypoproteinemia is associated with a high metabolic state that can lead to excessive protein loss.33 The loss of proteins impairs immunological functioning and is linked to more severe disease, rapid deterioration, and higher fatality rates.34 Lymphocytes play a central role in the immune response, influencing the outcomes of bacterial and viral infections, as well as the effectiveness of vaccines.35 Our study found that 14.20% (25 out of 176) of cases with low lymphocyte counts experienced mortality, while none of the cases with high lymphocyte counts resulted in death. The adjusted hazard ratio for the cohort with low lymphocyte counts was 2.01 (1.07–3.76) compared to those within the normal interval. This highlights the significance of lymphocyte counts as a prominent clinical feature for assessing the prognosis of COVID-19. Lastly, cases with co-infection of M. pneumonia predicted a higher risk of death compared to other cases. Although a meta-analysis suggested that 42% of bacterial co-infections in COVID-19 were caused by M. pneumonia,36 our cohort showed a lower prevalence of M. pneumonia co-infection at only 0.76% (4 out of 529). Nonetheless, M. pneumonia co-infection may exacerbate clinical symptoms and increase morbidity if left undetected or untreated.37 Therefore, active attention and timely treatment of M. pneumonia co-infections should be given during the treatment process, especially for elderly and infant patients.
Dyspnea, lymphopenia and hypoproteinemia are the three risk factors to death for COVID-19 patients. More than one-third of the patients simultaneously had both lymphopenia and hypoproteinemia (refer to Figure S3), which are immunocompromised conditions, and it may be reasonable to consider prophylactic treatment with broad-spectrum antibiotics for these susceptible patients. Correlation analysis indicated that lymphopenia is associated with the co-infection of H. influenza, and hypoproteinemia is associated with the S. pneumonia, H. influenza and P. aeruginosa. This result indicates a significant correlation between the co-infection of these bacteria and two key clinical indicators, namely hypoproteinemia and lymphopenia, closely associated with COVID-19 outcomes. This also further emphasizes the importance of controlling the occurrence of concurrent infections in the treatment of COVID-19 for prognosis.
Liminations
This study had several limitations that warrant consideration. Firstly, the analysis was confined to identifying co-infection patterns that could be detected within the bounds of the multiplex respiratory PCR panel. The scope of pathogen detection was limited to the selection of pathogens included in the panel, potentially overlooking certain co-infections, such as fungal co-infections, that were not covered. Secondly, it’s important to acknowledge that the detection of respiratory pathogens using qPCR does not conclusively confirm active infections; rather, it indicates the potential risk of co-infection. As such, the presence of pathogens might not always translate to ongoing infections, and caution is needed in interpreting these results solely as evidence of co-infection. Thirdly, differentiating whether the bacterial infections documented in this study originate from community-acquired or nosocomial sources presents a challenge. It is plausible that patients could have harbored the bacterial organisms prior to the onset of the viral infection. Fourthly, the vaccination status concerning pneumococci, Hib, and influenza among our patients is unavailable, precluding an assessment of these vaccines’ influence on co-infections in COVID-19 patients. Fifthly, our study lacks data from healthy or mildly affected COVID-19 groups as controls, hindering a comprehensive analysis of PCR methods’ clinical relevance in detecting COVID-19 co-infections and guiding treatment. Additionally, the detected pathogens might be associated with pre-existing chronic conditions or could have been acquired within a healthcare setting. This complexity underscores the need for nuanced interpretation when attributing the origin of bacterial infections.
Conclusions
This study involved qPCR analysis of respiratory specimens from 716 hospitalized COVID-19 patients during a surge in infections following the relaxation of public health measures in China. We screened for 12 common viral and bacterial respiratory pathogens and found that 76.82% (550/716) of cases were co-infected with at least one pathogen, with 44.73% (246/550) having two or more co-infecting pathogens. Among bacterial co-infections, S. pneumonia, Hib, and K. pneumonia were the most prevalent, while FluA, RSV, and Adenovirus were the most common co-infection viruses. Our study revealed discrepancies between the detection of bacterial co-infections and the prescription of antibiotics in some cases. Univariate and multivariate Cox proportional hazards regression analyses identified several covariates associated with an increased risk of death, including dyspnea, hypoproteinemia, low lymphocyte counts, and M. pneumonia co-infection. Vaccinating against co-infectious pathogens, such as pneumococcal, Hib, and influenza vaccines, constitutes an effective strategy in COVID-19 treatment. This approach helps prevent co-infections and enhances patient outcomes when health system capacities may be limited. Treatment guidelines that optimize respiratory support, nutrition, and selective antibiotic use can be beneficial, particularly for vulnerable patients with severe or complicated COVID-19. Overall, this study emphasizes the importance of understanding and managing co-infections in COVID-19 patients to enhance the quality of care and reduce mortality rates, especially in challenging healthcare situations.
Data Sharing Statement
All data analyzed and generated in this study were included in the manuscript and supplementary materials.
Ethics Approval and Consent to Participate
This work has been approved by the Ethics Committee of the Affiliated Hospital of Youjiang Medical University for Nationalities (Approval number: YYFY-LL-2023-119). This study employed a retrospective analysis of de-identified medical records, and no direct contact or interaction with human participants was involved. All clinical data of hospitalized COVID-19 patients data used were fully anonymized, and no personal identifiers were accessible to the research team. Thus, the ethics committee waived the requirement for consent. The study was conducted in accordance with the principles described in the Declaration of Helsinki, and the confidentiality of patients was guaranteed.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was funded by the Science and Technology Base and Talent Program in Guangxi (GuikeAD23026078). We also thanks for the support of Construction of Key Clinical Specialties in Guangxi (Guiweiyifa [2022]-NO.21) and the Key Laboratory of Molecular Pathology of Guangxi.
Disclosure
The authors declare no conflict of interest.
References
1. Zhu N, Zhang D, Wang W, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi:10.1056/NEJMoa2001017
2. Lazarus JV, Romero D, Kopka CJ, et al. A multinational Delphi consensus to end the COVID-19 public health threat. Nature. 2022;611(7935):332–345. doi:10.1038/s41586-022-05398-2
3. Ginsburg AS, Klugman KP. COVID-19 pneumonia and the appropriate use of antibiotics. The Lancet Global Health. 2020;8(12):e1453–e1454. doi:10.1016/S2214-109X(20)30444-7
4. Musuuza JS, Watson L, Parmasad V, Putman-Buehler N, Christensen L, Safdar N. Prevalence and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: a systematic review and meta-analysis. PLoS One. 2021;16(5):e0251170. doi:10.1371/journal.pone.0251170
5. Sreenath K, Batra P, Vinayaraj EV, et al. Coinfections with Other Respiratory Pathogens among Patients with COVID-19. Microbiol Spectr. 2021;9(1):e0016321. doi:10.1128/Spectrum.00163-21
6. Zhu X, Ge Y, Wu T, et al. Co-infection with respiratory pathogens among COVID-2019 cases. Virus Res. 2020;285:198005. doi:10.1016/j.virusres.2020.198005
7. Wang Z, Yu M, Lin L. The emerging antimicrobial resistance crisis during the COVID-19 surge in China. Lancet Microbe. 2023;4(5):e290–e291. doi:10.1016/S2666-5247(23)00038-1
8. Zhang H, Zhang Y, Wu J, et al. Risks and features of secondary infections in severe and critical ill COVID-19 patients. Emerg Microbes Infect. 2020;9(1):1958–1964. doi:10.1080/22221751.2020.1812437
9. Commission NH. Diagnosis and treatment plan for SARS-Cov2 infection (10th Edition). In: commission NH, ed. Available from: http://www.gov.cn/zhengce/zhengceku/2023-01/06/content_5735343.htm2023. Accessed October 20, 2023.
10. Lex A, Gehlenborg N. Sets and intersections. Nat Methods. 2014;11(8):779. doi:10.1038/nmeth.3033
11. Binbin S, Yannan L, Yaohua T, Chen C, Xiaoying Z. Confronting COVID-19 and Prioritizing Aging Population. China CDC Weekly. 2023;5(10):229–233. doi:10.46234/ccdcw2023.042
12. Jue L, Fan D, Yu W, et al. Trends of SARS-CoV-2 Infection in Sentinel Community-Based Surveillance After the Optimization of Prevention and Control Measures — china, December 2022–January 2023. China CDC Weekly. 2023;5(7):159–164. doi:10.46234/ccdcw2023.028
13. Kim E-H, Nguyen T-Q, Casel MAB, et al. Coinfection with SARS-CoV-2 and Influenza A Virus Increases Disease Severity and Impairs Neutralizing Antibody and CD4 T Cell Responses. J Virol. 2022;96(6):e0187321. doi:10.1128/jvi.01873-21
14. Wu HY, Chang PH, Chen KY, et al. Coronavirus disease 2019 (COVID-19) associated bacterial coinfection: incidence, diagnosis and treatment. J Microbiol Immunol Infect. 2022;55(6 Pt 1):985–992. doi:10.1016/j.jmii.2022.09.006
15. Guo L, Wei D, Zhang X, et al. Clinical Features Predicting Mortality Risk in Patients With Viral Pneumonia: the MuLBSTA Score. Front Microbiol. 2019;10:2752. doi:10.3389/fmicb.2019.02752
16. Moreno-Garcia E, Puerta-Alcalde P, Letona L, et al. Bacterial co-infection at hospital admission in patients with COVID-19. Int J Infect Dis. 2022;118:197–202. doi:10.1016/j.ijid.2022.03.003
17. Parker A, Jackson N, Awasthi S, et al. Association of upper respiratory Streptococcus pneumoniae colonization with SARS-CoV-2 infection among adults. Clin Infect Dis. 2022;76(7):1–9.
18. Carniel BF, Marcon F, Rylance J, et al. Pneumococcal colonization impairs mucosal immune responses to live attenuated influenza vaccine. JCI Insight. 2021;6:4.
19. Park JJ, Narayanan S, Tiefenbach J, et al. Estimating the global and regional burden of meningitis in children caused by Haemophilus influenzae type b: a systematic review and meta-analysis. J Glob Health. 2022;12:04014. doi:10.7189/jogh.12.04014
20. Hosoda T, Harada S, Okamoto K, et al. COVID-19 and Fatal Sepsis Caused by Hypervirulent Klebsiella pneumoniae, Japan, 2020. Emerg Infect Dis. 2021;27(2):556–559. doi:10.3201/eid2702.204662
21. Root-Bernstein R, Huber J, Ziehl A, Pietrowicz M. SARS-CoV-2 and Its Bacterial Co- or Super-Infections Synergize to Trigger COVID-19 Autoimmune Cardiopathies. Int J Mol Sci. 2023;24(15):12177. doi:10.3390/ijms241512177
22. Root-Bernstein R. Possible Cross-Reactivity between SARS-CoV-2 Proteins, CRM197 and Proteins in Pneumococcal Vaccines May Protect Against Symptomatic SARS-CoV-2 Disease and Death. Vaccines. 2020;8:4.
23. Nunes MC, Cutland CL, Klugman KP, Madhi SA. Pneumococcal Conjugate Vaccine Protection against Coronavirus-Associated Pneumonia Hospitalization in Children Living with and without HIV. mBio. 2021;12:1. doi:10.1128/mBio.02347-20
24. Pawlowski C, Puranik A, Bandi H, Venkatakrishnan AJ, Soundararajan VJSR. Exploratory analysis of immunization records highlights decreased SARS-CoV-2 rates in individuals with recent non-COVID-19 vaccinations. Sci Rep. 2021;11(1):1–20. doi:10.1038/s41598-021-83641-y
25. Swets MC, Russell CD, Harrison EM, et al. SARS-CoV-2 co-infection with influenza viruses, respiratory syncytial virus, or adenoviruses. The Lancet. 2022;399(10334):1463–1464. doi:10.1016/S0140-6736(22)00383-X
26. Li L, Wang H, Liu A, et al. Comparison of 11 respiratory pathogens among hospitalized children before and during the COVID-19 epidemic in Shenzhen, China. Virol J. 2021;18(1):202. doi:10.1186/s12985-021-01669-y
27. Bai L, Zhao Y, Dong J, et al. Coinfection with influenza A virus enhances SARS-CoV-2 infectivity. Cell Res. 2021;31(4):395–403. doi:10.1038/s41422-021-00473-1
28. Dee K, Schultz V, Haney J, Bissett LA, Magill C, Murcia PR. Influenza A and respiratory syncytial virus trigger a cellular response that blocks severe acute respiratory syndrome virus 2 infection in the respiratory tract. J Infect Dis. 2022.
29. Martínez-Baz I, Trobajo-Sanmartín C, Arregui I, et al. Influenza Vaccination and Risk of SARS-CoV-2 Infection in a Cohort of Health Workers. Vaccines. 2020;8:4.
30. Fink G, Orlova-Fink N, Schindler T, et al. Inactivated trivalent influenza vaccination is associated with lower mortality among patients with COVID-19 in Brazil. BMJ Evid Based Med. 2020. doi:10.1136/bmjebm-2020-111549
31. Chotpitayasunondh T, Fischer TK, Heraud JM, et al. Influenza and COVID-19: what does co-existence mean? Influenza Other Respir Viruses. 2021;15(3):407–412. doi:10.1111/irv.12824
32. Yeoh YK, Zuo T, Lui GC, et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut. 2021;70(4):698–706. doi:10.1136/gutjnl-2020-323020
33. Ambade V. Biochemical rationale for hypoalbuminemia in COVID-19 patients. J Med Virol. 2021;93(3):1207–1209. doi:10.1002/jmv.26542
34. Ali AM, Kunugi H. Hypoproteinemia predicts disease severity and mortality in COVID-19: a call for action. Diagn Pathol. 2021;16(1):31. doi:10.1186/s13000-021-01092-5
35. Castro Dopico X, Ols S, Loré K, Karlsson Hedestam GB. Immunity to SARS-CoV-2 induced by infection or vaccination. J Intern Med. 2022;291(1):32–50. doi:10.1111/joim.13372
36. Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020;81(2):266–275. doi:10.1016/j.jinf.2020.05.046
37. Fan BE, Lim KGE, Chong VCL, Chan SSW, Ong KH, Kuperan P. COVID-19 and mycoplasma pneumoniae coinfection. Am J Hematol. 2020;95(6):723–724. doi:10.1002/ajh.25785

