Cardiovascular
Severe asthma mortality rates appear slightly lower in US vs. Europe
October 25, 2023
3 min read
Key takeaways:
- 1.9% of the U.S. cohort died during the study period.
- 14% of reported deaths had a contributory COVID-19 diagnosis.
- Findings may indicate mortality risks in patients with severe asthma.
HONOLULU — Adults with severe asthma in the United States experienced a slightly lower mortality rate than prior data showed of similar patients in Europe, according to a poster presented at the CHEST Annual Meeting.
The most commonly reported cause of death was cardiovascular disease, Njira L. Lugogo, MD, MS, associate professor of internal medicine and director of the asthma program within the division of pulmonary and critical care medicine at University of Michigan Health, said during the presentation.
“There is a minimal amount of data out there about the mortality rate and cause of death in patients with severe asthma,” Lugogo told Healio.
Njira L. Lugogo
“We felt it was critical to understand what is contributing to mortality in severe asthma patients with the intention of identifying opportunities to change treatment paradigms to manage risks in this patient population,” she said.
In a previous European multinational study of patients with severe asthma conducted between 2008 and 2013, all-cause mortality estimates ranged between 11.3 and 14.8 per 1,000 person-years.
The ongoing, noninterventional CHRONICLE study comprises adults with severe asthma in the United States who are being treated with biologic therapy or maintenance systemic corticosteroids or whose asthma is persistently uncontrolled despite treatment with high-dosage inhaled corticosteroids.
The researchers investigated all-cause mortality incidence rates and investigator-reported primary causes of death among 3,574 patients (69% women; 73.5% white; average age at enrollment, 54.4 years) enrolled in CHRONICLE between February 2018 and November 2022, with an average follow-up per patient of 1.5 years.
There were 72 (2%; 65.3% women; 76.4% white) deaths reported, with an average age of 64.4 years at enrollment. The study incidence rate was 8.5 per 1,000 person-years (95% CI, 6.7-10.7).
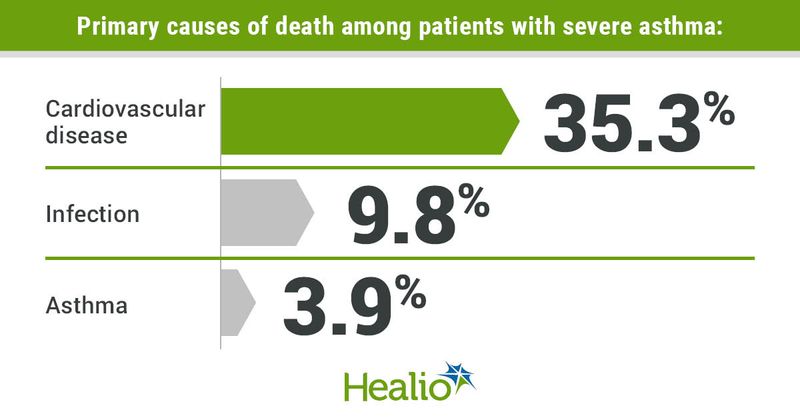
Of the 51 deaths with a reported cause, cardiovascular disease was the most common cause of death overall at 35.3%, including 13.7% due to heart failure and 21.6% from other cardiovascular disease.
“It was quite surprising that the primary cause of death in this population is cardiovascular disease, which is similar to COPD,” Lugogo said.
In COPD, she continued, cardiovascular disease is attributed to tobacco use and systemic inflammation.
“In asthma, it is likely that cardiovascular risk is tied to use of oral steroids that increases the prevalence of metabolic disease,” Lugogo said. “This is a topic we intend to explore further in our patient population.”
For example, Lugogo said, she and her colleagues believe that the impact of asthma on cardiovascular disease is likely not direct causality. Rather, she said that she and her colleagues are exploring the concept that oral corticosteroid exposure increases the incidence of metabolic comorbidities and, subsequently, this results in an increased risk for death of cardiovascular disease.
Also, infection accounted for 9.8% of deaths. A contributory COVID-19 diagnosis was part of 21.6% of deaths. Asthma was the cause of death in 3.9% of patients, which Lugogo called lower than national rates and unexpected. For 21.6%, the primary cause of death was reported as “other.”
“The expectation was that mortality would be attributed to asthma and respiratory failure, but that was not the case,” Lugogo said.
Another unexpected finding, Lugogo said, was that mortality rates were not higher in African American patients in the cohort, which is not consistent with national data.
“It is notable that the CHRONICLE study includes only patients in subspecialty care, which may explain that lack of a difference in mortality rate based on race,” she said.
These results may help identify mortality risks among patients with severe asthma, the researchers said, and may support future studies of connections between severe asthma and fatal cardiovascular disease.
“We need to embrace new treatment paradigms in asthma care where we identify high-risk patients and aggressively manage their disease early on, including escalating those that need biologics to treatment much faster as a means of oral corticosteroid sparing,” Lugogo said.
“We also need to screen our patients for cardiac disease and work on risk mitigation,” she said.
Next, Lugogo said that she and her colleagues will work on identifying the potential contributors to mortality in asthma and whether asthma therapies such as oral steroids are increasing mortality risk.
“In addition, we are interested in whether asthma patients are less likely to receive medications that are cardioprotective such as beta blockers because of their asthma, which may be putting them at increased risk,” she said.
Reference:
Sources/Disclosures
Collapse
Disclosures:
Lugogo reports having financial relationships with AKH, Amgen, AstraZeneca, Avillion, Genentech, Gossamer, GSK, Janssen, Medscape, NACE, Novartis, Regeneron, Sanofi and Teva. Please see the abstract for all other authors’ relevant financial disclosures.