Infection
Not implementing generic PrEP programs for young MSM would be ‘throwing away’ lives, money
November 06, 2023
2 min read
Key takeaways:
- PrEP adherence and engagement continues to be an issue for young men who have sex with men.
- PrEP use among this group, however, would reduce new infections and decrease costs.
Implementing generic PrEP programs for young men who have sex with men at risk for HIV — a group known to have adherence and engagement issues — would reduce new infections and be cost-effective, according to a study.
“It is critically important that preventive tools such as pre-exposure prophylaxis (PrEP) be made available to those who can benefit most from them. In the U.S., about 20% of new HIV diagnoses occur among youth aged 13 to 24 years, and young men who have sex with men (YMSM) account for 81% of the new diagnoses within this age group,” Anne M. Neilan, MD, an infectious disease specialist at Massachusetts General Hospital, told Healio.
“However, YMSM are less likely to access preventive tools such as PrEP, and if prescribed PrEP, they may also have difficulties adhering to PrEP and remaining engaged in PrEP programs,” Neilan said.
Because of this, she said, there are concerns about whether it is “worth the investment” to promote PrEP use among YMSM and whether it is a valuable use of resources given the known adherence and engagement challenges.
To better understand how tenofovir-based daily oral HIV PrEP would compare with currently recommended CDC-recommended annual HIV screening in terms of clinical benefits and costs, Neilan and colleagues used an adolescent-focused simulation model to compare annual HIV screening alone with tenofovir disoproxil fumarate/emtricitabine–based oral PrEP and every 3-month HIV screening in YMSM at increased risk of HIV.
According to the study, data used for the study included age-stratified HIV incidence/100 person-years (PY) on- or off-PrEP (0.6-10.1 or 0.4-6.4), PrEP retention at 6 years, transmissions by HIV RNA level (078.4/1,00 PY) and annual costs of ART ($32,000-$69,000), HIV care ($3,100-$34,600) and PrEP program/generic drug ($900/$360).
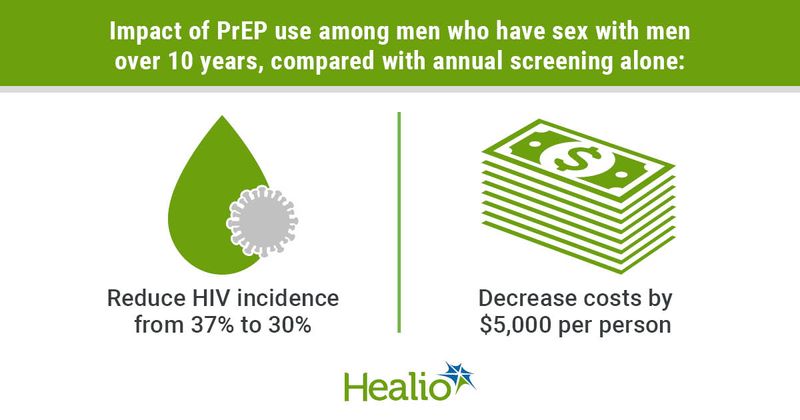
Overall, the study showed that PrEP use among YMSM aged 15 to 24 years would increase quality-adjusted life-years from 9.58 to 9.67, reduce new infections from 37% to 30%, and decrease costs by approximately $5,000 over 10 years compared with annual screening alone.
Additionally, the study showed that PrEP would remain cost-saving for HIV incidence off-PrEP 5.1/100 PY or more or with an annual PrEP price of $1,200 and under.
They added that over a lifetime, PrEP would be cost-saving for HIV incidence off-PrEP 1/100 PY or more across all retention assumptions assessed during the study. However, PrEP would not be cost-effective at HIV incidence 0.1/100 PY or less regardless of drug price “due to programmatic costs.”
“The study findings show that we would be throwing away both lives and money by failing to rollout generic PrEP programs for YMSM at increased risk for HIV acquisition. Indeed, efforts should be made to expand PrEP access to ensure we realize the benefits highlighted in this study,” Neilan said. “These findings are particularly important given the recent availability of generic tenofovir-based PrEP and recent national discussions concerning drug pricing.”
Sources/Disclosures
Collapse
Disclosures:
Neilan reports no relevant financial disclosures. Please see the study for all other authors’ relevant financial disclosures.