Cardiovascular
Trends in Cardiovascular Health Counseling Among Postpartum Individuals
Key Points
Question
What percentage of birthing adults in the US with prepregnancy cardiovascular disease risk factors or adverse pregnancy outcomes received cardiovascular health counseling at the postpartum visit from 2016 through 2020?
Findings
In a serial cross-sectional analysis of nationally representative data from the Pregnancy Risk Assessment Monitoring System, prevalence of self-reported postpartum counseling for healthy eating, exercise, and losing weight gained during pregnancy was approximately 60% and experienced small declines from 2016 through 2020 among individuals with prepregnancy cardiovascular disease risk factors or adverse pregnancy outcomes.
Meaning
At-risk individuals may not be receiving cardiovascular health counseling at their postpartum visit.
Importance
Poor prepregnancy cardiovascular health (CVH) and adverse pregnancy outcomes (APOs) are key risk factors for subsequent cardiovascular disease (CVD) in birthing adults. The postpartum visit offers an opportunity to promote CVH among at-risk individuals.
Objective
To determine prevalence, predictors, and trends in self-reported CVH counseling during the postpartum visit.
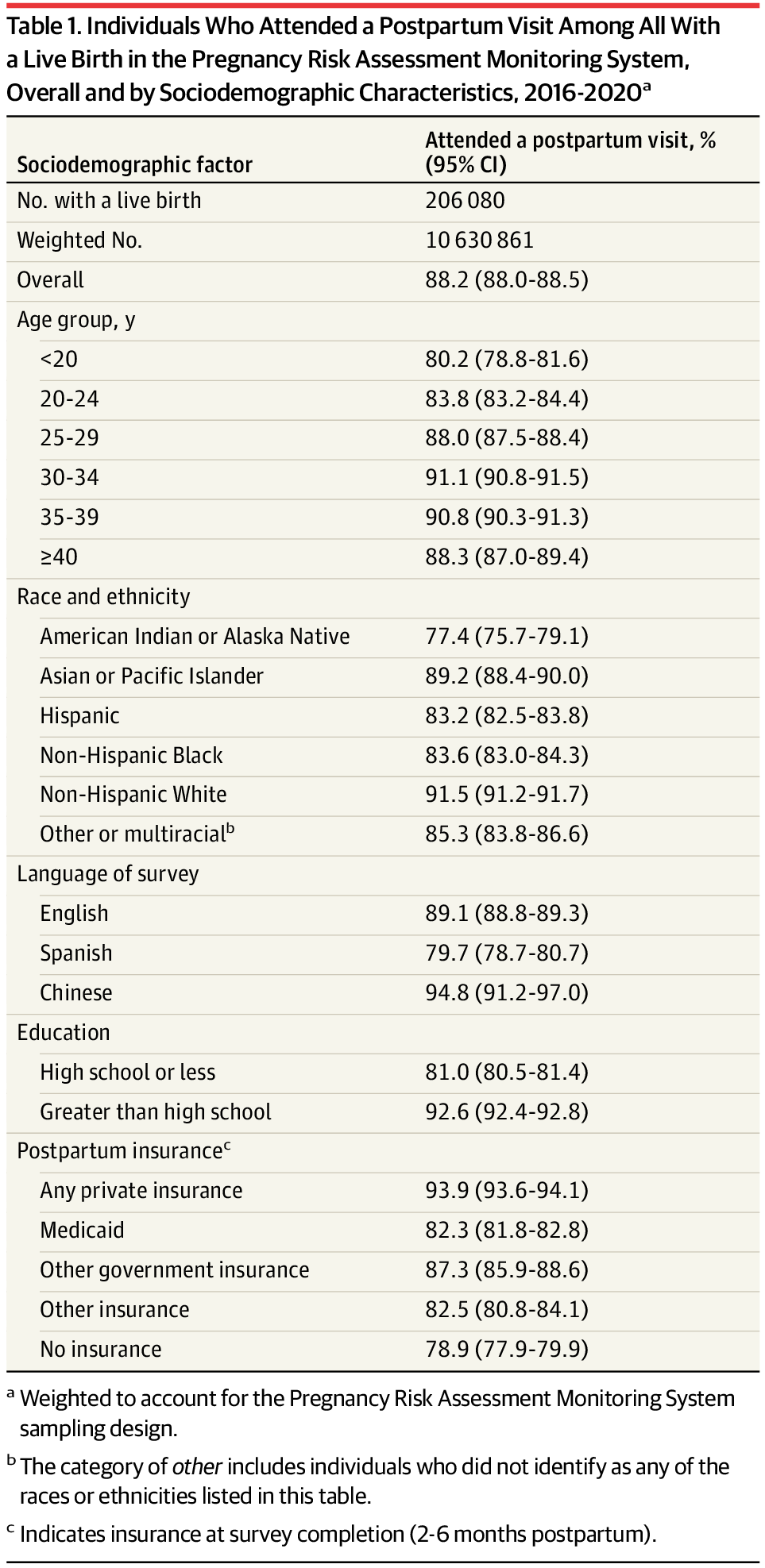
Design, Setting, and Participants
Serial, cross-sectional analysis of data from 2016-2020 from the Pregnancy Risk Assessment Monitoring System (PRAMS), a nationally representative, population-based survey. The primary analysis included individuals who attended a postpartum visit 4 to 6 weeks after delivery with available data on receipt of CVH counseling, self-reported prepregnancy CVD risk factors (obesity, diabetes, and hypertension), and APOs (gestational diabetes, hypertensive disorders of pregnancy, and preterm birth) (N = 167 705 [weighted N = 8 714 459]).
Exposures
Total number of CVD risk factors (0, 1, or ≥2 prepregnancy risk factors or APOs).
Main Outcomes and Measures
Annual, age-adjusted prevalence of self-reported postpartum CVH counseling per 100 individuals, defined as receipt of counseling for healthy eating, exercise, and losing weight gained during pregnancy, was calculated overall and by number of CVD risk factors. Average annual percent change (APC) assessed trends in CVH counseling from 2016 through 2020. Data were pooled to calculate rate ratios (RRs) for counseling that compared individuals with and without CVD risk factors after adjustment for age, education, postpartum insurance, and delivery year.
Results
From 2016 through 2020, prevalence of self-reported postpartum CVH counseling declined from 56.2 to 52.8 per 100 individuals among those with no CVD risk factors (APC, −1.4% [95% CI, −1.8% to −1.0%/y]), from 58.5 to 57.3 per 100 individuals among those with 1 risk factor (APC, −0.7% [95% CI, −1.3% to −0.1%/y]), and from 61.9 to 59.8 per 100 individuals among those with 2 or more risk factors (APC, −0.8% [95% CI, −1.3% to −0.3%/y]). Reporting receipt of counseling was modestly higher among individuals with 1 risk factor (RR, 1.05 [95% CI, 1.04 to 1.07]) and with 2 or more risk factors (RR, 1.11 [95% CI, 1.09 to 1.13]) compared with those who had no risk factors.
Conclusions and Relevance
Approximately 60% of individuals with CVD risk factors or APOs reported receiving CVH counseling at their postpartum visit. Prevalence of reporting CVH counseling decreased modestly over 5 years.